Anthem Blue Cross won’t accept automatic credit card payments anymore
- Share via
Most businesses are eager to have people pay their monthly bills with automatic credit card payments. There’s a good reason: Businesses know they will get paid on a regular basis.
So why is health insurance heavyweight Anthem Blue Cross telling members it will no longer allow them to do this — at least not without a hefty fee?
Tom Harris of West Los Angeles has been insured by Anthem for about 40 years. He’s paid his bills automatically from his credit card account for as long as he can remember.
“It’s much simpler this way,” Harris, 60, told me. “I never have to worry about writing a check.”
But he received a notice from Anthem the other day informing him that automatic card payments will be discontinued Aug. 1. “We reviewed our processes and decided to eliminate this payment method,” the company explained.
Anthem also is eliminating the option of making payments on a bimonthly or quarterly basis. Beginning Aug. 1, all payments will have to be made monthly.
So what are Harris’ choices? Anthem says he can continue paying with plastic, but he’ll have to call a service rep each time. This will result in a $15 “convenience fee” every time Harris pays his bill.
To make payments without additional charges, Anthem says, members can either send in checks each month or register online to have money automatically withdrawn from their checking accounts.
But — and this is a big but — anyone who now makes automatic card payments will start receiving monthly statements from Anthem. This will result in a $2 fee each month, which others who aren’t on automatic payment plans already are charged.
Anthem says it will waive the $2 fee for a while so members can adjust to the new system. “We will let you know before the $2 fee returns,” it says.
So let’s recap: Anthem is doing away with a practice that most other businesses prefer for its customers’ convenience and guaranteed payments, and will instead charge a $15 monthly fee if you want to keep using your credit card.
Even if you switch to paying by check, you’ll still be charged $2 a month to receive a paper statement that you didn’t ask for.
As Harris put it: “That’s $24 a year just to pay your bills. It seems crazy.”
Or highly profitable. Anthem, after all, has more than 8 million members in California.
On top of that, think of all the airline miles and rewards points Anthem members will lose by not paying premiums with plastic — unless they also want to pay an extra $180 a year in convenience fees.
So what does the company say? Not much.
Leslie Porras, an Anthem spokeswoman, merely reiterated the contents of the company’s notice to members when I asked about the new billing practices. She declined to comment on the rationale for the changes.
In the absence of a better explanation, I’m inclined to see things the way Harris sees them: Anthem is making a money grab.
Perhaps the insurance giant is trying to deter use of credit cards so it won’t have to pay processing fees to the likes of Visa and MasterCard. Perhaps it sees some additional benefit in being hooked into people’s checking accounts.
The bottom line is that it’s making customers pay to pay, and that’s unacceptable. At the very least, Anthem should arrange for free electronic statements to be issued so people could avoid the costly paper statements they never wanted in the first place.
Seriously, health insurers don’t think they get enough bad press already?
Buy this drug
Speaking of healthcare, reader David Eisen contacted me over the weekend with a couple of urgent questions. The first involved why the prizes in Cracker Jack boxes aren’t cool anymore. Sadly, I have no answer for that one.
The other question involved those ubiquitous ads on TV and in print for prescription drugs. “Would you really want to go to a doctor to whom you had to suggest a medication?” Eisen asked.
If you put it like that, the answer for most people is probably no. But the drug industry wants consumers to at least ask for costly name-brand drugs, rather than settle for cheaper generics.
Believe it or not, only two countries allow pharmaceutical companies to pitch prescription drugs directly to consumers: the United States and New Zealand. All other nations view this as an inappropriate intrusion on the relationship between doctor and patient.
In 2007, drug makers spent nearly $5 billion on so-called direct-to-consumer ads, according to a recent study by the University of Pennsylvania’s Leonard Davis Institute of Health Economics.
More than 80% of doctors say these ads result in patients’ requesting specific medications, and they often will accommodate these requests to keep patients happy, the study found.
Although the study didn’t address this, you can be sure the pharmaceutical industry isn’t swallowing the billions spent on marketing prescription drugs. Those costs are passed along to consumers in the form of higher prices for medicine.
Direct-to-consumer drug ads were prohibited in the United States until 1997, when the Food and Drug Administration decided to give it a whirl. Since then, marketing of prescription drugs has exploded, making a night of TV seem like an endless catalog of disorders and side effects.
From 1999 to 2009, the number of prescriptions purchased in the United States increased 39%, while the population grew only 9%, according to the Kaiser Family Foundation. And most prescriptions written were for newer, more expensive drugs.
On the brighter side, at least you don’t have to pay a convenience fee for using your credit card at the drugstore.
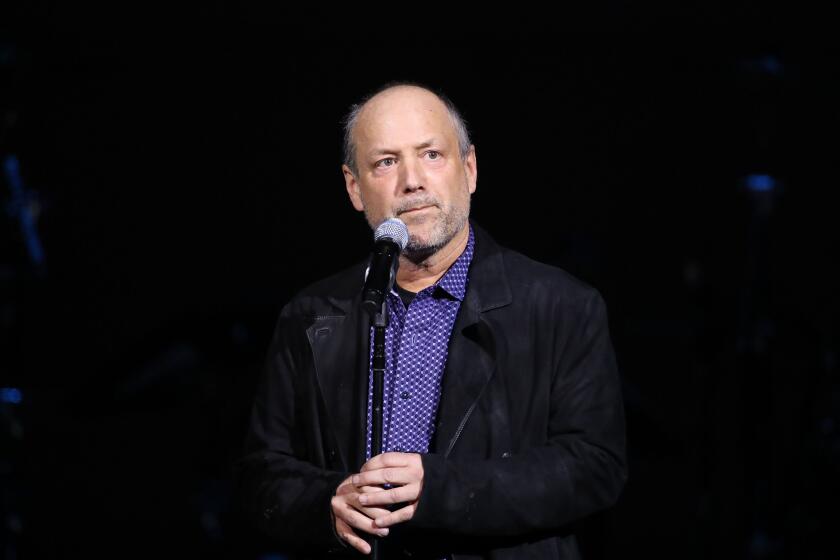
David Lazarus’ column runs Tuesdays and Fridays. He also can be seen daily on KTLA-TV Channel 5. Send your tips or feedback to david.lazarus@latimes.com.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.