UnitedHealth Group sues California over fine
- Share via
Setting up a major legal fight, UnitedHealth Group Inc. has sued California’s insurance commissioner to block his attempt to fine the insurer $173.6 million for violations during a botched 2005 acquisition.
The lawsuit, filed Thursday in Orange County Superior Court, is the latest twist in a long-running political drama. Four years ago, California sought a jaw-dropping fine of nearly $10 billion against UnitedHealth, the nation’s largest insurer. The penalty related to problems handling medical claims and policyholder applications after the insurer bought Cypress-based PacifiCare.
But that record penalty didn’t stand. Last year, an administrative law judge rejected much of the state’s case and said UnitedHealth should be fined no more than $11.5 million.
Last month, California Insurance Commissioner Dave Jones rejected that ruling in a 220-page decision and imposed the $173.6-million penalty. He ordered UnitedHealth to pay it by July 22.
That drew the lawsuit and a fiery response from UnitedHealth executives Thursday. The insurer, based in Minnetonka, Minn., said Jones was abusing his power and setting a dangerous precedent by seeking such stiff punishment for relatively minor violations.
“This ruling threatens to paralyze the healthcare system in the state, resulting in more costs and bureaucracy for Californians,” said Stephen Scheneman, president of UnitedHealth’s PacifiCare unit. “We are taking this action to protect the interests of our customers, who depend on the availability of affordable health insurance.”
Byron Tucker, a spokesman for the insurance department, said the agency hadn’t had time to fully review UnitedHealth’s lawsuit.
But he said, “Commissioner Jones carefully applied the law, and the department is confident the penalty will withstand the lawsuit.”
In its June 9 decision, the insurance department said its proposed fine “appropriately reflects the gravity of PacifiCare’s offenses and provides the necessary deterrent effect going forward.”
The handling of the case by Jones, a Democrat running for reelection, could become a point of contention in this fall’s campaign over health insurance rate regulation. An initiative on the November ballot would give the insurance commissioner the authority to reject health insurance rate increases that he deems unreasonable.
Health insurers, business groups and other opponents say the ballot measure gives the insurance commissioner too much power and subjects the rate-setting process to politics.
Jones has said rate regulation is crucial to protect consumers and small businesses from excessive rate hikes. He also says the rate regulation authority is essential to fulfill the goals of the Affordable Care Act.
UnitedHealth has long acknowledged that the takeover of PacifiCare didn’t go as planned. The company admits numerous mistakes in processing medical claims and customer applications.
California initially took action against UnitedHealth in 2008 under then-Insurance Commissioner Steve Poizner, a Republican. At first, he said a fine of $1.3 billion was warranted.
Two years later — while Poizner was seeking the Republican nomination for governor — he upped the ante and sought as much as $10 billion in penalties. To justify the enormous fine, insurance regulators said UnitedHealth committed more than 900,000 violations after taking over PacifiCare.
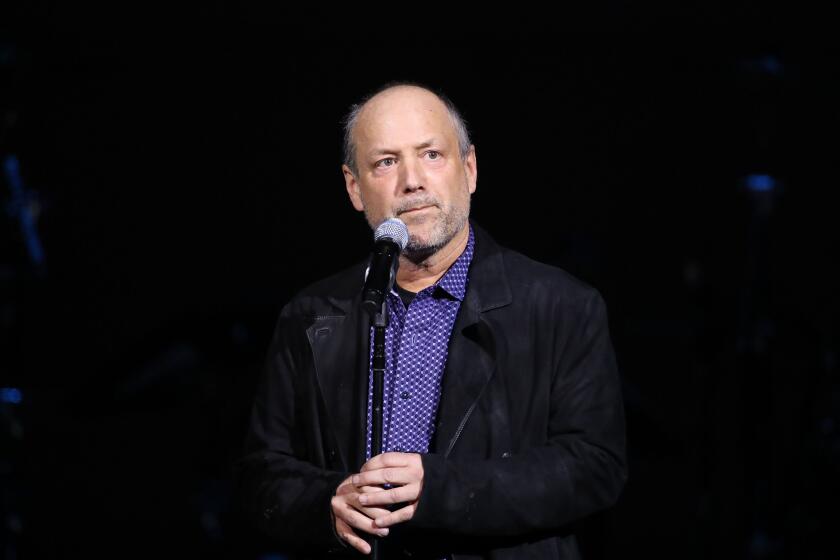
Thursday, Poizner stood by his aggressive pursuit of the case while he was in office. He declined to comment directly on the latest developments.
“When companies come to California and acquire healthcare organizations, and do not keep promises made to the California Department of Insurance and the people of California, there should be stiff fines,” Poizner said. “In my opinion, that’s what happened when UnitedHealth Group bought California-based PacifiCare.”
Poizner is now chief executive of EmpoweredU, an education technology company in Campbell, Calif.
UnitedHealth had challenged Poizner’s proposed fines with an administrative law judge. The case dragged on from December 2009 to June 2013, and the state judge heard testimony and arguments for more than 230 days.
The state insurance department has already agreed to pay nearly $10 million to outside lawyers to litigate this case, records show.
In her August 2013 decision, Administrative Law Judge Ruth S. Astle found that “there were numerous problems related to the integration” of UnitedHealth and PacifiCare. She noted significant problems receiving, tracking and retrieving paper documents submitted to PacifiCare.
PacifiCare identified 1,799 claims that it had denied in 2006 because of its failure to verify existence of previous coverage, court records show.
“This is a serious violation in that it left some claimants with no coverage,” the judge wrote. “It is difficult to assess the full impact since some claimants may have given up and just waited out the six-month exclusion.”
The administrative law judge, in setting her $11.5-million fine, noted that the insurer failed to pay claims correctly or on time.
The judge’s ruling was more in line with other penalties assessed against health insurers. The state’s other insurance regulator, the Department of Managed Health Care, cited many of the same problems and reached a settlement with UnitedHealth for a $2-million fine.
Twitter: @chadterhune
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.