New ways to fight bacteria
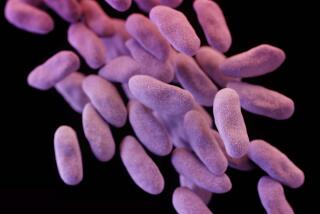
Doctors and infectious bacteria are locked in an arms race. In this ever-escalating battle, the bacteria evolve ways to avoid every drug humans throw at them.
The conflict has intensified lately as more and more bacteria — particularly those lurking in hospitals — become able to resist nearly every antibiotic in our arsenal.
“We throw thousands and thousands of antibiotics on bacteria,” says Marcin Filutowicz, a microbiologist at the University of Wisconsin in Madison. “This is tremendous selection for antibiotic-resistant bacteria.”
The situation is forcing scientists to think creatively about where the next antibacterial medications will come from and how they will work. Here are five provocative ideas.
Viruses
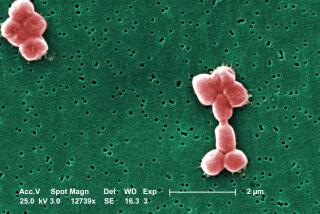
Humans aren’t the only ones who suffer infections. Bacteria, too, can get infected by viruses — and the enemies of our bacterial enemies are, naturally, our friends. These viruses, called bacteriophages or simply phages, are harmless to people but deadly to bacteria.
Scientists first discovered phages in 1917. But when scientists figured out how to make and use penicillin in 1941, Western doctors dropped phage treatments.
On the other side of the Iron Curtain, however, phage therapies remained popular, says Alexander Sulakvelidze, a microbiologist who grew up in what is now the nation of Georgia.
“Almost everyone that I know in Georgia has taken phages at one time or another,” Sulakvelidze says. He is the chief scientist at Intralytix Inc., a Baltimore-based company he founded to exploit phages for human benefit.
In recent years, Western scientists have rekindled their interest in phage treatments, and their experiments show the viruses cure bacterial infections in animals. In a 2009 study, published in the Journal of Wound Care, researchers at the Southwest Regional Wound Care Center in Lubbock, Texas, confirmed the safety of Intralytix’s viruses on 42 people with chronic leg ulcers.
Since 2006, a few food processing companies have enlisted phages to prevent contamination in their facilities. Intralytix’s ListShield infects and kills Listeria monocytogenes, a bacterium that can cause deadly cases of food poisoning.
“The beauty of this is that it’s 100% natural, it’s not corrosive, it’s not harsh,” Sulakvelidze says. If you wanted to, “you could drink it.”
It should be difficult for bacteria to evade phages by evolving resistance. “The phages, being biological entities, really will evolve along with the infection,” says Roy Sleator, a microbiologist at the Cork Institute of Technology in Ireland.
Pharmabiotics
Not all bacteria are bad. A person normally carries around more than four pounds of bacteria that not only don’t cause disease, but also help prevent it by taking up space and resources.
Scientists are trying to harness these friendly bacteria to fight off their disease-causing brethren that do manage to get a foothold. This approach is based on the “probiotics” in the yogurts and other products at the grocery store, but Sleator is taking it to the next level by improving those probiotics in the lab. He calls these souped-up microbes “pharmabiotics.”
Sleator has created bacteria that are better able to colonize the gut, where they fight listeria infection. In a 2008 study in the journal BMC Microbiology, Sleator reported that mice that ate the supercharged pharmabiotics before swallowing listeria had fewer listeria bacteria in their bodies than mice that ate regular probiotics.
Next, Sleator would like to make his pharmabiotics produce drugs that attack the bad bacteria directly — either by poking holes in their cell walls or neutralizing the toxins they produce. He is also working to ensure that the engineered bacteria could not run rampant in the world at large.
“If they ever find themselves out in the external environment, outside of a treatment setting, they cannot survive,” he says.
But inside the body, pharmabiotics can, like phage, evolve in step with disease-causing bacteria, so it should be hard for the bad bacteria to dodge the treatment.
Filutowicz, too, is toying with good bacteria that can seek out the nasty ones and either pump them full of antibiotics or force them to produce the antibiotics themselves. He founded a company, ConjuGon Inc., to develop his ideas. In a 2007 paper in the Journal of Burn Care & Research, Filutowicz reported that his pharmabiotics successfully knocked down infection and promoted survival in mice with infected burns.
Weird places
Many current antibiotics come from bacteria or fungi that need to fight off neighboring microbes. Now, scientists are casting a wider net in their search for new antimicrobial agents — including looking in animals, such as frogs, that are very good at fighting off bacteria.
Michael Conlon, a chemist at the United Arab Emirates University in Al-Ain, invites colleagues to send him samples of the chemicals frogs secrete on their skin so he can test their antibacterial activity.
“People think I’m some kind of lunatic,” Conlon says. “Why on earth would you ever look in frog skin for antibiotics?”
The reason is that frogs live in warm, wet environments, making their skin an appealing home for bacteria. So frogs have evolved an arsenal of bacteria-killing chemicals to protect themselves.
At the August meeting of the American Chemical Society in Boston, Conlon reported that he has amassed a collection of skin secretions from more than 6,000 kinds of frogs. He has found more than 100 frog slime compounds that attack bacteria. “They just rip big holes in the cell membrane,” Conlon says.
Fighting off the frog bactericides will require larger evolutionary changes than bacteria needed to resist current antibiotics, so it should take a while before they manage to resist the new drugs.
Conlon is not the only scientist thinking beyond the ordinary in his hunt for new antibiotics. Frog skin sounds positively reasonable compared to what scientists at the University of Nottingham in the U.K. are exploring. At the September meeting of the Society for General Microbiology in Nottingham, Simon Lee presented work on antimicrobials he and colleagues found in the brains of cockroaches and locusts.
The bugs, after all, live in pretty dirty environments and need to prevent infection. The researchers found that the insect tissues killed more than 90% of the bacterium methicillin-resistant Staphylococcus aureus, better known as MRSA.
The immune system
While some scientists look outward, other scientists are looking inward at how the human body naturally fights infection. At the September Interscience Conference on Antimicrobial Agents and Chemotherapy in Boston, scientists discussed a new kind of antibiotic based on human defensive weaponry that destroys the bacteria’s membrane.
Because the membrane is such a complex part of the cell, it is unlikely that bacteria will quickly evolve ways to disable or avoid the drugs, says Richard Scott, vice president for research at PolyMedix Inc. in Radnor, Pa.
PolyMedix is designing chemicals that mimic the shape and action of bacteria-fighting proteins called defensins. They hope to target MRSA, for which only a couple of antibiotics are now effective.
PolyMedix researchers have already shown that their pseudo-defensin treats infections in animals. The drug appeared safe in a trial involving 77 healthy people; the main side effect was a tingling in the fingers and toes. The company hopes to soon test the drug in people with MRSA infections, Scott says.
Disarming
Menachem Shoham, a biochemist at Case Western Reserve University in Cleveland, isn’t interested in killing bacteria such as MRSA. He hopes to simply disarm them.
Staph bacteria are quite common. In fact, Shoham says, one-third of us live comfortably with harmless staph in our bodies. But occasionally, those harmless bacteria start to produce toxins that destroy blood cells and cause disease.
Shohan is focusing on a bacterial gene, called AgrA, that bacteria need to make toxins. He has found a handful of compounds that block AgrA and protect blood cells, he reported at the ICAAC meeting.
Shoham’s idea is to use these drugs not to stop the infection but to decrease its severity. Then, he expects, the patient’s immune system can take over and cure the disease.
The drugs wouldn’t kill the bacteria, so there’s little incentive to develop resistance, Shohan says.
Ongoing battle
But ultimately, bacteria will come up with a way to beat even the most clever of human drug designers.
“As long as we are on this planet,” Filutowicz says, “we will need new ideas and new antibiotics to confront bacteria.”
health@latimes.com