Revulsion to War Isn’t a Mental Disorder
- Share via
A recent study, led by military psychiatrist Charles Hoge, concluded that more than 1 in 6 combatants are leaving Iraq with a mental health problem.
In a commentary in the New England Journal of Medicine accompanying the findings, Matthew Friedman of the Department of Veterans Affairs and the National Center for Post-Traumatic Stress Disorder ominously warned that these figures might even “underestimate the eventual magnitude of this clinical problem.”
So does all this suggest there’s an emerging epidemic of chronic mental disorder among those returning from Iraq? Not necessarily. In fact, the study may have overestimated the problem.
First, consider how the researchers assessed for possible psychiatric illness: They asked members of four combat infantry units to anonymously complete questionnaires on symptoms of depression, generalized anxiety and post-traumatic stress disorder about three or four months after they returned to the United States. People with the disorder experience nightmares, startle reactions, insomnia and disturbing thoughts about the trauma. Of 1,692 infantrymen, 12.6% checked off enough disabling symptoms to suggest a diagnosis of post-traumatic stress disorder.
But any mental health professional knows that a questionnaire can only suggest a diagnosis, not confirm one. A diagnosis of post-traumatic stress disorder requires a structured interview by either a psychiatrist or clinical psychologist. Ticking off items on a checklist may simply reflect normal expressions of distress rather than symptoms of a serious mental illness. Certainly, participants in this study witnessed many horrors and experienced intense combat. It is little wonder that some remain distressed several months later. But that’s not the same as post-traumatic stress disorder.
Furthermore, although it’s true that 12.6% of the combatants seemed to meet the criteria for post-traumatic stress disorder after returning from Iraq, 5% of those who completed the questionnaire apparently had already met criteria for the disorder before leaving for Iraq, according to the study.
Does this mean that nearly half of the cases are attributable to traumatic events that occurred before these individuals left the United States? Or, as is possibly the case, does it mean that the questionnaire is measuring nonspecific distress, not symptoms of post-traumatic stress disorder per se?
Finally, even if you believe the 1-in-6 ratio, the study tells a story of resilience as much as mental disorder. In fact, the rate of post-traumatic stress disorder is far lower than previous research would have led us to expect.
For example, the congressionally mandated Vietnam Veterans Readjustment Study done in the late 1980s estimated that 30.9% of all men who served in that war developed post-traumatic stress disorder, even though only about 15% had been assigned to combat units. Hoge’s research team investigating Iraq war veterans reported a much lower rate despite confining their study to personnel assigned to combat units.
To emphasize resilience is not to minimize suffering. The sheer intensity of combat in Iraq guarantees that many veterans will need cognitive-behavior therapy, medication or both for their post-traumatic stress disorder.
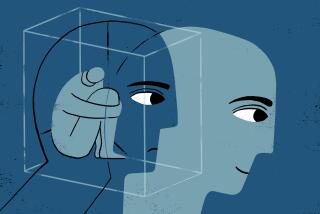
Our veterans deserve the best treatment we can provide, promptly and confidentially. At the same time, we must be wary of pathologizing normal human responses to an inhuman situation. Intense emotional responses to horrific events are common, and they signify mental disorder only when they fail to wane with time.
Richard J. McNally, a psychology professor at Harvard University, is the author of “Remembering Trauma” (Harvard University Press, 2003).
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.