40-plus years as a pediatrician
In more than 40 years as a pediatrician, I’ve worked in the military, in a small private practice and in a large multi-specialty group. And I’ve seen huge changes, both in administrative practices and in treatment protocols.
Many of the changes have been just short of miraculous. When I was training to be a pediatrician in the late 1960s and early ‘70s, I visited wards filled with cases of childhood meningitis — a very serious condition that can lead to death or lifelong neurological complications.
Today, with immunizations available against two of the most common causes of meningitis, I can’t remember the last time I hospitalized a child with this illness, but it has to have been more than 20 years ago.
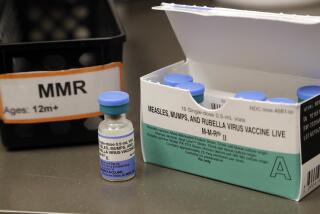
In my early years of practice, I also saw cases of measles, rubella and whooping cough, and, of course, almost all children developed chickenpox. Today, there are immunizations against all these diseases, so it is uncommon to see them.
But that could change. A new wave of uninformed, anti-vaccine sentiment is persuading some parents to forgo or delay immunizing their children. The science is clear-cut: Vaccines save lives, and serious side effects are exceedingly rare. Will it take a new wave of children dying from whooping cough or other preventable diseases to turn the tide? I wish that parents reluctant to vaccinate would talk to their grandparents before deciding against immunizations.
Another big step forward involves asthma treatment. During the first two decades I practiced, children with asthma were hospitalized frequently. Today, we have far better medications and better treatment protocols that are keeping asthma patients out of hospitals.
In another area, I’m hoping we have finally learned that less treatment is sometimes better than more. When I was being trained, pediatricians were taught to use antibiotics only when necessary, but that lesson wasn’t fully embraced and many doctors prescribed the medications when they weren’t called for. This was due to a number of factors: patient pressure, fear of having missed a diagnosis that would call for antibiotics, and time constraints. (Sometimes, it’s faster to write a prescription than it is to explain why antibiotics are unnecessary.)
But this widespread use of antibiotics has led to bacterial resistance, and we are now paying the price. Fortunately, the pendulum has finally swung back to a more judicious use of these agents.
Sadly, there are some conditions involving adolescents that have increased in incidence over the years. Forty years ago, I seldom saw a teenager with anxiety, depression or attention-deficit disorder. Today, these things are weekly occurrences. My colleagues and I also see a lot more childhood obesity.
Part of the uptick we are seeing in these conditions may be that we are more diligent about diagnosing them than in the past, but that can’t totally explain the marked increase. We need to figure out what is causing the rise and address it. Are there things parents can do? Schools? Physicians?
Drug use by some teenagers has been a constant during my years in practice. The popularity of a drug rises and falls as teenagers chase the latest craze, but drug abuse was a problem when I entered pediatrics and it remains one. Sometimes drugs are used to self-medicate other emotional problems. Sometimes kids use drugs simply because others are doing it.
Today, for better or worse, there seems to be greater acceptance of marijuana use. It’s hard to say what effect that will have in the long run. But I can say from long experience that the adolescents I see who are heavy marijuana users are often not very successful in school
Another trend since I entered medicine is the rise of alternative treatments. Do they work? It’s hard to say because most of these therapies haven’t undergone rigorous testing. But I’d wager that there is more snake oil being sold today than there was a century ago.
Perhaps the most frustrating change in medicine has been the recent embrace of electronic medical records. I see the potential benefits of this technology, but its implementation is far too burdensome. Every physician I know complains that electronic charting has decreased productivity, increased frustration and taken away precious time for communicating with patients.
Despite all the changes, positive and negative, the most basic part of being a pediatrician remains the same. The essence of medicine is to connect and communicate with patients in order to understand and meet their health needs. It’s about developing a trusted relationship over time. But it is also about seeing an infant grow into a vibrant teenager and then into a confident young adult. It’s about seeing a second generation as former patients return with their children. Patients are not consumers or clients, and medicine is not just a job. Being a physician is still an honor and a privilege.
Richard Buchta is a pediatrician at Scripps Clinic in San Diego.
Find additional essays in the Labor Pains series. Has your work changed in recent years? Tell us about it by email at laborpains@latimes.com or on Twitter at #latlaborpains.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.