Op-Ed: Vaccine hesitancy is common among Black healthcare workers. We’re trying to resolve it

Across the nation, Black healthcare workers are receiving the COVID-19 vaccine at rates far lower than their white counterparts. We have seen this disparity in our own health system, Penn Medicine, where during the first two weeks of vaccine rollout, just 22% of eligible Black employees, compared with 62% of eligible white employees, got vaccinated or signed up to receive the shot.
As Black physicians, we were alarmed but not surprised. While we have been vaccinated, we each made the decision with varying levels of uncertainty.
Health systems across the country, and particularly those with large numbers of Black employees, must have an intentional and coordinated strategy to address vaccine hesitancy. The objective is not to coerce or convince. The goal is to ensure that Black staff members have accurate information that addresses common vaccine misconceptions — and the opportunity for dialogue in a nonjudgmental setting.
Consistent with many health systems across the country, the majority of employees in support service roles at Penn Medicine are people of color whose jobs do not involve regular interaction with physicians or other healthcare providers. There are few informal opportunities for spontaneous conversations, a structural barrier that is often overlooked when all health system employees are lumped into one group.
We sought to change that. As Black leaders at Penn Medicine, we recognized our unique position to address our community directly: to own the past mistakes of the medical profession, acknowledge present-day racism in healthcare and offer an opportunity for conversation about the vaccine with trusted messengers. In partnership with our health system, we developed a multimodal educational outreach approach about COVID-19 and the vaccine, Operation Caveat.
This racist history in rural Alabama has had lasting implications on how Africans Americans view healthcare in America.
We urge other healthcare leaders to adopt similar strategies to meet people where they are — literally and metaphorically.
Our goal was to reach staffing groups with a high percentage of Black employees, including environmental services, food services, patient transport and materials management. Operation Caveat targets the places where these employees regularly spend time, enlisting the following strategies.
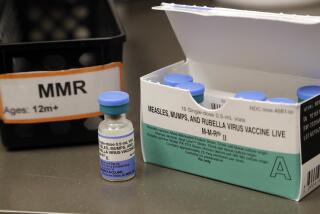
Printed material featuring Black physicians. We developed a one-page handout with photographs of five Black physicians who have received the COVID-19 vaccine and included their reasons for deciding to get vaccinated. Also featured are facts about the vaccine that address concerns we had heard from staff. For example, some were concerned that the vaccine is a live virus and could give them COVID-19; others were concerned about side effects. Handouts were distributed to support staff along with vaccine sign-up information, thus addressing email access barriers as well.
Rolling PowerPoint presentation in high-traffic staff areas. A PowerPoint slide presentation highlighting COVID-19 myths and facts, interspersed with testimonials from a diverse group of employees who have received the vaccine, plays on screens in staff break rooms. The slide show takes on myths such as “the vaccine causes Bell’s palsy” and “the vaccine was rushed to market.” Each myth is followed by information from the Centers for Disease Control and Prevention that debunks it or addresses the concern. The presentation is now a screensaver on monitors throughout the hospital.
Daily huddles with physicians and staff groups that have a high proportion of Black employees. Pairs of physicians attended daily staff huddles to share their vaccination experiences and answer questions about the vaccine. Each physician pair had at least one Black member. In one week, 13 huddles that each lasted about 30 minutes reached about 240 staff members. The huddles were videotaped so other staff members could access the information discussed.
The huddles provided an opportunity to address legitimate concerns face-to-face. The physicians provided information on how the COVID-19 vaccines were developed, details on how they work and the expected side effects. Staff were reassured that Black scientists have been involved in the vaccine development process and that the safety and efficacy findings were applicable to people of all races and ethnicities.
Initial feedback from the huddles suggests they are having an impact. The chance to ask questions of medical personnel addresses hesitations that are often the result of mistrust rooted in historical and present-day experiences of racism. Our vaccine center administrators have reported that some Black staff members told them they decided to get the vaccine after physicians personally talked to them about it.
With the COVID-19 vaccine rollout, health systems across the country are asking Black staff to have faith in a system that has not always acted in trustworthy ways when it comes to Black and other marginalized communities. Black physician leaders have a vital role to play in the efforts to overcome legacies of mistrust by leveraging our scientific knowledge base, teaching skills and concern for our community. Our Black staff needs to hear from Black experts. The unfortunate reality is that there are too few of us in medicine, underscoring the importance of efforts to diversify the physician workforce.
Outside the walls of the hospital, our Black employees are trusted messengers for their families, friends and neighbors. As the vaccine becomes more widely available, these networks will be a vital part of ensuring that Black communities have the information they need to decide to get vaccinated. If we do not reach those who are understandably hesitant, the crisis of COVID-19 racial disparities will only widen.
The authors are affiliated with Penn Medicine. Dr. Florencia Greer Polite is chief of the Division of General Obstetrics and Gynecology. Dr. Eugenia C. South is a senior fellow at the Leonard Davis Institute of Health Economics. Also contributing to this op-ed article are Dr. Abike T. James, vice chair for Inclusion, Diversity and Equity in the Department of Obstetrics and Gynecology, and Dr. Nwamaka D. Eneanya, a senior fellow at the Leonard Davis Institute of Health Economics.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.