The Unwanted Challenge : AIDS Specialists Say Fear, Ignorance Make Doctors Unwilling to Deal With Patients in the Epidemic
- Share via
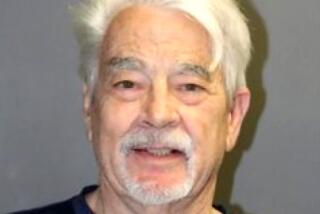
Dr. Sherman Williamson, a family physician in Orange, has been treating people infected with acquired immune deficiency syndrome since early on in the AIDS epidemic.
Thirty of his patients have died, and he is now treating “at least 50” who have tested positive for the human immunodeficiency virus (HIV) that causes AIDS.
It is not a medical specialty Williamson sought out. It developed because he was willing to treat AIDS patients and to learn more about the disease--a willingness that appears to have set him apart from many of his colleagues.
Although AIDS patients--and gay men at risk--have long complained about the difficulty of finding informed, compassionate medical care, recent statistics add weight to their argument:
--According to a random sampling of Los Angeles County physicians done last year by the County Medical Assn., only about a fourth of the doctors surveyed said they were interested in treating AIDS patients or felt competent to do so.
--In a 1987 study of physicians in Sacramento, 35% said they would not care for AIDS or HIV-positive patients; an additional 15% were undecided.
--In a recently completed American Medical Assn. study on physician knowledge and attitudes about AIDS, 91% of the physicians surveyed said that medical doctors should take a leadership role in addressing AIDS, but “80% felt that their professional colleagues were not completely prepared to deal with AIDS patients.”
Such statistics, coupled with the personal experiences of many HIV-positive patients, have contributed to a rising tide of complaints by AIDS specialists: that doctors don’t want to treat AIDS patients because it is disheartening work, that many physicians are ill-informed about the symptoms and course of AIDS and therefore fail to diagnose it when aggressive treatment would make the most difference, and that doctors in general are uncomfortable asking questions about life style and sexual orientation--a squeamishness that can have life-threatening consequences for patients at risk.
These problems are only being compounded, many critics say, as the numbers of HIV-positive people across the nation increases. (According to the latest government estimates, 365,000 people will be diagnosed with AIDS by Jan. 1, 1993.)
AIDS specialists say that although there are certainly numerous physicians across the country who have responded in a positive, responsible and caring way to the disease, there simply aren’t enough of them.
“Many doctors think that AIDS will never touch their doorstep,” said Dr. Constance B. Wofsy, co-director of AIDS programs at San Francisco General Hospital. “There is such a denial process. Many feel that the AIDS specialists must be the ones to deal with it.”
From traveling with colleagues, Wofsy said she has noticed that the trend in any given city is for a small group of physicians to take on care of HIV patients.
“There is an expectation that those doctors will deal with it,” she said. “In general, many doctors feel it is someone else’s problem.”
“It is an avoidance phenomenon,” said Sherman Oaks AIDS specialist Dr. Joel Weisman, who, with Dr. Michael Gottlieb, reported the first cases of AIDS in Los Angeles in June, 1980. “In an ideal world, every physician should treat the patient with AIDS. In the real world, that’s just not going to happen.”
In Los Angeles, Dr. Martin Finn, director of the AIDS program for the Los Angeles County Department of Health Services, says that he knows of no more than 100 doctors who are caring for AIDS patients in this area.
“And they tend to cluster around hospitals with AIDS units,” he said. “I think one of the things we’re seeing here is a new subspecialty. And what we will be seeing in the next year is another cadre of subgroup, because we’re moving toward the use of the antivirals (antiviral medicines to treat the disease).
“There aren’t enough people who know how to use them, so we’ll have to rotate patients through the immunologists and allergists.”
Williamson, an Orange County practitioner for 10 years, said he has already had difficulty getting specialists to assist him as consulting physicians in treating AIDS patients. So, over the years, he has developed his own network of referral physicians, cardiologists, gastrointestinal specialists and pulmonologists who are willing to do so.
“I call first myself, because it’s only appropriate that the physician make the contact,” he said. “Some will just tell me, ‘I would prefer not to.’ (But) I would rather have them turn me down than (turn down) the patient,” said Williamson, who admitted he is sensitive about his patients being rejected.
“Too many have been told to seek treatment somewhere else. But there are no somewhere elses in some places.”
“As a physician, I am truly embarrassed by the response of so many of my fellow physicians,” said Dr. Neil Schram, an internist at Kaiser who sees many HIV patients and is a member of the Los Angeles County Medical Assn.’s AIDS committee.
“Some physicians have done a heroic job, but the average physician has chosen to try to sit out this epidemic.”
Such indifference is particularly counterproductive, according to many AIDS specialists, now that so much more is known about strengthening the immune system. They point out that early detection of HIV infection is imperative because early treatment--such as with AZT, currently the most promising drug used against AIDS--seems to be a key in prolonging patients’ lives.
Schram, an outspoken advocate of AIDS education for doctors, insists that more physicians must take sexual histories of their patients and do far more counseling of patients whether or not the patients have tested positive for HIV.
“If you ask a question in a sensitive way, you can get the information without offending anybody,” he said. “As long as you’ve done it in a sensitive and caring manner.”
AIDS specialists note that if physicians don’t ask patients about their sexual orientation--and according to a recent Times survey, most do not--they may not advise a possibly high-risk patient to be tested for exposure to HIV. And symptoms can mean different things, depending upon a person’s sexual orientation. A persistent cough, for instance, might be a sign of HIV infection in a homosexual or bisexual man; less likely so in a heterosexual.
Doctors Can Counsel About Sex
By knowing a patient’s sexual history, they add, the doctor can counsel the patient on the importance of “safe sex” in the prevention of HIV infection.
“It bothers me that we can’t treat AIDS like any other disease. But we aren’t,” said Williamson. “People come to me and they’re not getting adequate treatment because the doctor didn’t know what to do.
“And there are other problems. There’s a lack of knowledge. . . . Of course, homophobia is part of it. And then there’s the fear of an unknown illness.”
Most observers agree that AIDS patients, the majority gay men or intravenous drug users, have faced serious problems of homophobia among doctors since the disease was discovered among homosexuals.
Doctors Uncomfortable With Gays
In a 1986 study of California primary care physicians conducted by Dr. Charles Lewis, professor of clinical medicine at UCLA, the state’s doctors did not score well in their level of knowledge about AIDS, and they expressed considerable reluctance in treating gay patients.
One-third of the 1,000 doctors surveyed statewide said that they were uncomfortable dealing with gays.
“I know in my heart how much emotions get in the way,” Lewis said. “But there’s probably no such thing as scientific values in an emotional vacuum. We have mostly ignored this emotional context of decision making (in medicine). All the facts get embedded in molasses when you talk about AIDS.”
Physicians Will Face Decision
“As time goes by, more practicing physicians will be faced with the decision whether to treat HIV patients,” said Dr. Peter Wolfe, a UCLA infectious diseases specialist who treats many HIV patients.
“Most probably reasonable people will. But there is no lack of crazy people in the medical profession as in anything else. People who are unable to make a rational, appropriate response. People who have the same fears and worries as anyone else, even though they were trained in analytical response and are men and women of good reason and intelligence.
“Surgeons are certainly the people in the front line,” Wolfe said. “They have the highest risk because they are exposed to blood products more than anybody else. . . (But) the reassuring thing about this disease is that we now have a knowledge of its history and epidemiology. We know enough about the virus to protect ourselves from it.”
Dr. Steven Short, a head and neck surgeon in Century City, follows the universal precautions--protective clothing--set down by officials from the Centers for Disease Control since AIDS was discovered, but he said, “We have to treat these people. We can’t turn them away.
“I operated on a man and I knew he had AIDS. I was very careful, but I got blood on my finger,” Short said. “I washed it off, but I can’t underestimate the significance of that. We have to be exquisitely careful. But we have to do the operation, too.”
Worry About Spouses
Short and other surgeons also cite the worry for their wives and husbands.
“My wife is a health educator and we’ve talked about the risks in surgery,” Short said. “She’s maybe a little concerned and I don’t think she likes it, but she knows I have to do it.”
Although Wolfe doesn’t believe in requiring patients to be tested for the HIV virus before surgery, Dr. Lorraine Day, chief of orthopedic surgery at San Francisco General Hospital, is an outspoken surgeon on the other side of that debate. Day and other orthopedic surgeons at General routinely ask patients to take HIV tests before operating on them.
Day does not refuse to operate on HIV-positive patients, she said, but she insisted her reason for testing is to have pre-operative knowledge about her patient’s HIV status.
Cuts Common, Surgeon Says
“I am concerned about myself and for my family,” Day said in a telephone interview. “I want to know what I am dealing with. We get cut all the time because of the tools we use, like carpenter’s tools. They are asking me to take risks and I want to know what the risks are.”
Some physicians treating AIDS patients report that they have had difficulties with partners in their own practice. One Los Angeles doctor who did not want his name used said that his partners had asked him to give up treating AIDS patients because they were afraid they might lose many of their other patients if the patients knew AIDS patients were treated there.
“Logic is not driving this (physician reaction to AIDS),” said Judith Ross, who teaches medical ethics at UCLA and chairs a Los Angeles group of health care professionals and educators on ethics and AIDS.
“People are functioning on a non-logical basis. . . . We may understand their fears, and their biases, but we can’t sanction their acting on those feelings. In the past they cared for patients with polio, tuberculosis and hepatitis B.
Doctors Pretend It Will Go Away
“The reaction (among physicians) now is to pretend we are going to get out of this in a month, or in three years. But that’s not going to happen. There are people who simply cannot get a doctor and that shouldn’t be.
“Society says to doctors, ‘We give you a monopoly profession, you govern yourselves and we provide resources to train you. In turn, you treat society.’ We cannot accept their abandoning the social contract that we have with them.”
Most AIDS specialists believe that the key to better and more compassionate medical treatment of HIV infected patients has to be education.
Weisman and his group have set up their practice as a model for educating doctors in AIDS treatment, and have had residents, interns, medical students and family practitioners come through their clinic to learn to treat AIDS patients firsthand.
Teaching AIDS Basics
Gottlieb, now in private practice and serving as an AIDS consultant to other physicians and their patients, is currently teaching “the basics of AIDS” to family practice residents at Santa Monica Hospital Medical Center.
There also are proposals in the works for medical schools to increase the time and material for medical students to learn to treat HIV patients as part of their training. And the state Legislature is considering a bill that would require physicians to be competent in treating HIV patients to be recertified to practice.
“There’s no question more educational efforts have to be directed toward physicians,” said Dr. Don Nielsen, an infectious disease specialist at Kaiser Permanente on Sunset Boulevard.
“Some physicians are certainly poorly informed, others simply don’t believe the information available, that you can’t get it by using the same phone as someone with AIDS. Doctors are not immune to the same reactions as the general public. But that’s where education comes in. They should know the resources and be able to treat the patients.
“There’s no question about the prejudice. We’ve been dealing with groups historically stereotyped--gays, bisexuals and i.v. drug users,” Nielsen said, explaining that the bulk of his practice is now HIV-infected patients, about 450 of them.
“But a person must be able to overcome that bias and treat the patients. I had no plans that this would be part of my practice, but who knew?”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.