Pressure Mounts to Let Consumers Sue HMOs
Life was draining out of 40-year-old cancer patient Rhonda Bast by the time her medical insurer finally agreed to approve a potentially life-saving bone marrow transplant.
That approval came too late. The cancer had spread to Bast’s brain, rendering futile the expensive and high-risk procedure. Bast’s hopes of staying alive for her toddler son had evaporated a few months earlier when her health plan refused to approve the treatment.
After her death, Bast’s family realized they could not hold the firm, Prudential Insurance Co., accountable.
“Unfortunately, without action by Congress, there is nothing we can do to help the Basts and others who may find themselves in this same unfortunate situation,” a federal appeals panel in San Francisco said in an opinion earlier this year.
The Basts’ case and others like it have propelled efforts by state and federal lawmakers to strip health plans of an immunity from certain types of lawsuits.
Most people are unaware of the Employee Retirement Income Security Act, or ERISA, which bars nearly 125 million Americans from collecting damages from their health insurers, including managed-care plans, for denial of medical treatment that results in death, injury or economic loss. ERISA allows people to recover only the benefits they were entitled to in the first place--for example, the cost of a cancer treatment. Many patients have difficulty finding lawyers to take such cases because the potential damages recovered are not enough to justify the expense of a lawsuit.
The 1974 federal law applies to those who get their health benefits through their employers; it doesn’t apply to government employees, those who buy individual medical policies, or those covered by Medicare, Medicaid or other government health programs.
A Growing Effort to Change the Law
Trial lawyers and patient advocates have argued for years that the law is outdated because the way in which health care is delivered and paid for has changed drastically in the last 25 years. Now there is a growing push by federal and state legislators to overhaul the law to allow consumers to sue their health plans--and their employers. And recently, federal judges across the country have voiced their own frustration with their inability, under ERISA, to punish HMOs and insurance companies for misconduct.
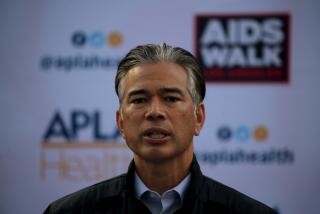
“The health plans use ERISA as a means of hiding behind decisions to deny care,” said state Assemblyman Martin Gallegos (D-Irwindale), who has proposed legislation that would allow consumers to sue HMOs.
Congress is also considering a number of bills that would allow consumers to bring lawsuits against health insurers and employer health plans. Perhaps the most sweeping of those bills is one sponsored by Rep. Charlie Norwood (R-Ga.). The Norwood bill, strongly opposed by insurance and business interests, has bogged down in a House committee.
Health insurers and business groups are lobbying hard to defeat federal or state legislation that would increase their liability. They claim the laws will expose them to a flood of litigation, raise medical premiums and force employers to drop coverage.
“The present system works well, and allowing damages to be levied against health plans or employers is not going to assure that the benefits themselves will be delivered,” said Mark Ugoretz, president of the ERISA Industry Committee, which represents many of the nation’s largest employers.
Consumer rights activists disagree.
“HMOs now have a get-out-of-jail-free pass,” said Jamie Court, director of Consumers for Quality Health Care, a Santa Monica watchdog group. “If HMOs don’t fear large damage awards, they will never approve expensive procedures like cancer treatment. Why would bank robbers stop stealing if all they had to do was give back what they stole?”
Patient advocates say Congress could not have anticipated the explosion of enrollment in managed-care plans when it passed ERISA 25 years ago.
In fact, ERISA was intended to establish uniform federal standards to enable companies operating in many states to offer the same health insurance plan to all employees without having to cope with a multitude of state laws and regulations. But when the Supreme Court interpreted the law in 1987, it held that ERISA barred consumers and their relatives from recovering damages.
Since then, the health-care system itself has changed radically with the rapid growth of HMOs and other managed-care plans, which now cover about 80% of all workers who get medical insurance through their employers.
Insurance companies and HMOS now routinely claim immunity under ERISA when they are sued for denying benefits to patients.
Across the nation, patients and their survivors have been left with no legal recourse against these insurers and HMOs. Among dozens who have been barred from suing are:
* A Denver man whose wife died after her HMO refused to pay for a bone marrow transplant for her leukemia.
* A New Orleans woman whose 8-month-old fetus died after an insurance company refused to approve her hospitalization for a high-risk pregnancy.
* A Boston woman whose 41-year-old husband, according to a federal judge, “never received the treatment he desperately required, suffered horribly and ultimately died needlessly” because his insurer refused to approve alcohol rehabilitation treatment.
Judge Cites Need for Action by Congress
In ruling after ruling, federal judges say they have no choice but to dismiss such suits against insurers and HMOs because ERISA demands it.
One Reagan appointee, U.S. District Judge William R. Young, who presided in the Boston case, said the HMOs’ denial of service “becomes another illustration of the glaring need for Congress to amend ERISA to account for the changing realities of the modern health-care system.”
Patient advocates say under ERISA, HMOs have no incentive to pay for expensive treatment because they cannot be held liable for damages.
“They are free to overturn doctors’ decisions with complete impunity. And if a patient dies, the HMO benefits by not paying” for the treatment, said Court, of the Santa Monica watchdog group.
A similar argument persuaded Texas Gov. George W. Bush last year not to veto a law that allowed patients to sue their health plans for malpractice--the first such law in the nation.
The Texas law went into effect last September, and so far not a single claim against an HMO has been filed.
One reason for the lack of lawsuits, legal observers say, is that the law applies only to malpractice claims involving actions that took place after September 1997. Malpractice cases typically take a year or longer to be filed.
Court and others say the Bast case highlights how insurance companies unduly benefit from ERISA.
Rhonda Rae Fleming Bast, mother of a 2-year-old son, was the manager of a Sears optical department in Seattle when she was diagnosed with breast cancer in December 1990.
Her left breast was removed the next month, but in August 1991, she was diagnosed with another cancerous growth in her left lung. Bast’s oncologist recommended that she undergo a bone marrow transplant or else she would surely die.
But Prudential officials declared that the procedure was not covered because it appeared to be “experimental in nature.” In February 1992, after Bast’s attorney showed Prudential that several other insurance companies had been ordered to pay for the procedure, the firm reversed its decision.
It was too late. The cancer had metastasized to Bast’s brain. She died in January 1993.
After a federal judge dismissed the suit against Prudential, Bast’s brother, attorney Michael Fleming, appealed to the U.S. 9th Circuit Court. In a decision issued last month, a three-judge panel said ERISA dictated that the suit be dismissed. The judges noted that other federal appellate courts “have reached the same conclusion under equally tragic remedies.”
Peggy Frank Lyle, a spokeswoman for Prudential, acknowledged that the firm initially denied Bast the bone marrow transplant because “it was generally considered experimental.”
“Our coverage position evolved in line with the prevailing opinion of the medical community and we began providing coverage for her specific condition in early 1992,” Lyle said in a statement.
Virginia Edin, Bast’s 71-year-old mother, said that five years after her daughter’s death, she still feels vengeful: “I would like to know where the people who made this decision that [denied] my daughter coverage live and I would like to do the same thing to their children and see what their reaction is.”
Edin said Douglas remembers little of his mother but knows about her experience with Prudential. “Whenever he hears any mention of “insurance company,” he stops and says, ‘Grandma, they killed my Momma.’ ”
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.