Leap From Animals to Humans
ATLANTA — It appeared at first we’d dodged the bullet. Now it’s not so clear. Monkeypox, a close cousin to the smallpox virus, unexpectedly appeared this month in the Midwest, far from its natural home in the rain forests of Congo, Liberia and Sierra Leone. For the last couple of decades, monkeypox in Africa has been an elusive threat. It has erupted in Congolese villages after someone has become infected through killing, skinning and eating a rat, squirrel or monkey. Sometimes the disease has been passed on to the victim’s family or fellow villagers and sometimes it hasn’t. Experts from the Centers for Disease Control and Prevention and other health officials have been telling us that monkeypox isn’t a very infectious disease. The truth, however, is a bit more complicated.
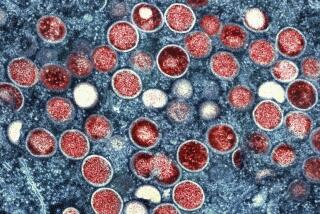
To understand why, we have to look at the biology of the disease. Unlike smallpox, monkeypox isn’t a human specialist. It’s an animal disease, and no one is sure what range of animals it infects. It kills monkeys, hence the name. Someone once found a dead squirrel on a Congo highway with suspicious-looking lesions on its skin. It turned out to have died of monkeypox, so some scientists decided that the disease is more a rodent disease than a primate disease. Apparently the disease infects giant Gambian rats, and now we know that prairie dogs, frequent victims of plague and tularemia, also can die from African monkeypox.
What has emerged from the remarkably rapid and effective investigation into the Midwest monkeypox outbreak is that African rodents, unsurprisingly, are the source of the disease. It appears that one giant Gambian rat, infected with monkeypox and housed with prairie dogs in a pet store, transmitted the disease to the prairie dogs, which were sold and swapped across several states.
Up to 68 people as of Friday had been infected. In the great bulk of those cases, the affected people appeared to have had direct contact with a sick pet. What doctors are more concerned about is person-to-person transmission, which indicates a more virulent strain, one better adapted to humans. At least three possible cases of monkeypox have now been found in people not exposed to animals. In Congo, where the death rate is up to 10%, monkeypox often spreads from person to person -- in part, public health officials say, because of primitive conditions.
But there’s more to it than that. In the Congo province of Kasai-Oriental, where monkeypox occasionally breaks out, people inhabit fairly large, airy huts within a family compound, which is usually some distance from other compounds. These are not such terrible conditions for keeping the disease in check. We can’t automatically assume, as some health experts contend, that it is better sanitation and living conditions in America that are keeping monkeypox from being so deadly here. Several other factors, hidden and not so hidden, are also at work.
As Peter Jahrling, the army’s chief virologist, explains it, monkeypox, like other diseases, is not a single strain; there are lots of variants. Like all forms of life composed of DNA or RNA, the monkeypox virus is subject to evolution, mutation, the force of natural selection. Whatever afflicted that Gambian rat, it probably wasn’t a single pure strain but a swarm of variants. And some of those strains possessed the ability to transmit from animals to people. We don’t know yet whether some of the strains also were capable of spreading from human to human, but that would not be surprising given what we know about the disease in Africa. It is the inevitable logic of natural selection at work: Those variants that are best at transmitting to people will be the ones that make the jump from animal to human. Then, among those strains, those even better at transmitting might jump again from human to human. This is a sort of winnowing-out process, where the best jumpers win.
In one well-documented outbreak in Congo, the chain of person-to-person monkeypox transmission was seven links long. If it hadn’t stopped moving, whether through medical intervention or because it ran out of hosts in the village, the disease would have become better and better at spreading among people. It would have become a more “humanized” disease.
It would have looked more and more like smallpox.
What would make a monkeypox germ a good jumper? Putting it simply, the virus has to do something to its host so it can get out of one human body and into the next. Some viruses, like measles, cause sneezing. Polio is passed in the stool and spread through the process unattractively known as “fecal/oral contact.” Monkeypox, like smallpox, has two such methods. As evolutionary biologist Paul W. Ewald, author of the well-known “Plague Time,” puts it, smallpox and monkeypox are “sit-and-wait pathogens”: Viral particles shed from the pox wait outside the body for the next host to happen by. These particles can last a long time in the external environment. Smallpox scabs kept on a shelf in a researcher’s office contained live, infectious virus after 13 years!
But smallpox, a highly evolved human disease, has another property that monkeypox sometimes has and sometimes hasn’t. This is the capacity to form sores or lesions in the throat. Such a sore, called an enanthema, is one of the chief ways smallpox spreads, particularly since these sores are formed before the patient gets terribly sick. You can walk around coughing and sneezing, infecting many people, before the disease knocks you off your feet. (This is why biodefense experts fear the so-called suicide cougher scenario for a smallpox attack.)
Only one person in this monkeypox outbreak appeared, at this writing, to have suffered from such enanthema. A young man in Indiana had to be taken to the emergency room because of sores in his throat. In Wisconsin, said epidemiologist Charles Edmiston, no enanthema had been found. This suggests that the particle salad of monkeypox strains brought over (apparently) by the giant Gambian rat may not have been particularly virulent at the outset, but we can’t be certain that will remain true. If human-to-human transmission is confirmed, it is likely that the disease will gain in virulence and transmissibility as it passes from one person to another.
The precautions taken by health departments in Milwaukee and elsewhere have helped to slow the spread of the disease, and their epidemiological investigations have been admirable. But the story is not over yet, and we should not be complacent.
Even if this outbreak is controlled quickly, the next time someone is foolish enough to pluck a wild African animal out of its natural habitat and ship it to the United States to entertain some animal fancier too jaded for a dog or cat or hamster, the strains might include some variants even better suited to human spread. To keep diseases out of this country, we must remember that it is not just people who transmit deadly human infections. Animals do as well.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.