Not-so natural selection
BIOPSIES are a pain. When they’re medically necessary we put up with them. When they’re not, most of us would just as soon remain un-punctured.
When the patient is a 3-day-old embryo, it’s especially fair to ask for some evidence of a clear medical benefit.
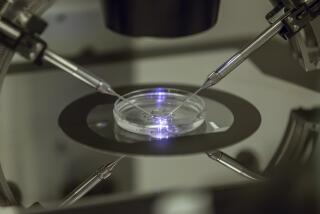
Pre-implantation genetic diagnosis, or PGD, is a procedure sometimes performed in conjunction with in vitro fertilization to improve the quality of the embryos selected. It entails the careful isolation of one of a 3-day-old embryo’s eight or so cells, then analysis of that cell’s genetic contents. Based on what is found, IVF patients and doctors can decide which embryos to transfer into the woman’s uterus.
Use of PGD has risen exponentially since its inception 17 years ago. In the U.S., where PGD isn’t formally tracked, about 3,000 procedures were performed in 2005, according to a recent report from the Genetics & Public Policy Center, which is affiliated with Johns Hopkins University. Experts estimate its frequency is rising annually by 15% to 30%.
In Europe, where more accurate numbers are available, a reporting system found a more than 20-fold jump in PGD procedures between 1999 and 2003, the most recent year for which figures are available.
But specialists are concerned that much of the rise in PGD is for an unproven goal: improving the successful pregnancy rates of older women undergoing IVF. “There’s a lot of controversy in the field as to how PGD should be appropriately applied,” says Catherine Racowsky, director of the IVF lab at Boston’s Brigham and Women’s Hospital.
Virtually everyone in the fertility community agrees that PGD is valuable for its original use: preventing the transmission of certain serious inherited disorders. But many are far less confident about use of the costly procedure on the embryos of otherwise healthy mothers whose only problem is the decline in fertility that inevitably comes with advancing age.
Experts say there is a lack of solid evidence that PGD results in an actual increase in the so-called “take-home baby rate.”
They say the procedure mostly makes sense for women who have experienced repeated miscarriages while undergoing in vitro fertilization and want to avoid any more of them.
Some experts also harbor suspicions that, just maybe, removing a cell from an early-stage embryo could be harmful, although there is not much evidence to support such a fear.
Performed for the original medical reasons, PGD works wonders. The first reported PGD procedures, published in the journal Nature in 1990, prevented transmission of serious genetic disorders caused by a defective gene on one of the mother’s two X chromosomes. Such disorders almost exclusively affect boys because a girl has two copies of the X chromosome and, to get the disease, both would have to carry a defective copy of the gene. Researchers successfully selected healthy offspring by sex-typing single cells from early embryos (by determining if they had two X chromosomes or one X and one Y) and then transferring only female embryos to the mother’s womb.
*
Expensive diagnosis
Since then, advances in molecular biology have allowed more detailed analysis of the DNA of embryos. Today, embryologists can hunt for mutations in single genes responsible for rare but deadly disorders such as Tay-Sachs disease or cystic fibrosis. This isn’t cheap: Parents who are at risk of transmitting severe single-gene disorders but wouldn’t otherwise need to use IVF, could easily spend $25,000 for the procedure. Still, for at-risk couples, shrinking the 25% or 50% prospect of an embryo’s inheriting a debilitating disease often makes PGD worth it.
But recent surveys show that in about two-thirds of the cases, PGD isn’t being used to detect genetic diseases. It’s done, instead, to inspect embryos created in the lab for abnormal chromosome counts in cases in which parents with fertility problems are already undergoing IVF.
Such abnormal counts -- sometimes an extra chromosome, other times a missing one -- are far more common in the case of older mothers and can lead to higher rates of miscarriage and birth defects. The goal of PGD is to improve healthy-pregnancy rates by screening out embryos whose cells are carrying extra or missing chromosomes, before transferring them to the mom’s uterus. The biopsy (removal of the cell) and subsequent analysis add about $3,000 to the cost of IVF.
Some practitioners, such as veteran researcher Yuri Verlinsky, director of the Chicago-based Reproductive Genetics Institute, maintain that PGD should be performed routinely for all IVF patients to help increase the success rate.
But growing numbers of specialists think PGD is being oversold -- and hopeful parents may be spending thousands without any increase in their chances of taking home a baby.
On face value, the idea of screening for extra or missing chromosomes (a condition known as aneuploidy) made sense: “The concept was that if you screen embryos’ genetic contents before you select them for transfer, you’re more likely to pick the correct ones,” says Dr. Richard Scott, founder and managing partner of Reproductive Medicine Associates, a large chain of IVF centers in the Northeast.
*
Benefits in question
The trouble is that studies so far have not borne out the early promise of this idea, he says. A carefully-controlled Belgian study published in the journal Human Reproduction in 2004 found no improvement in full-term pregnancy rates for about 150 would-be mothers age 37 or older whose embryos underwent aneuploidy screening compared with a roughly equal number of women who didn’t. In fact, the PGD group had fewer successful pregnancies (19) than the control group (29).
And a study conducted by Scott (reported at American Society for Reproductive Medicine’s annual meeting last October) had a similar, negative result on about 120 younger women (ages 32 to 38). Pregnancy rates were the same whether embryos were screened or not. If anything, Scott says, the non-PGD group did slightly better.
Why no improvement? For one thing, although screening out embryos with observed chromosomal anomalies can mean fewer miscarriages, it doesn’t increase the number of viable embryos available for transfer into an older woman’s uterus. Compared with a younger woman, an older woman produces relatively few eggs -- perhaps half a dozen per round of IVF -- all of which can, in practice, be put in her uterus. Rejecting any of them due to a diagnosis of aneuploidy just reduces the total number transferred.
Practitioners are very reluctant to transfer an embryo that’s diagnosed as abnormal via PGD, says Barry Behr, director of Stanford University’s IVF laboratory, if only because it would leave them open to lawsuits. Yet there’s reason to believe that some of those screened-out embryos could have implanted successfully and developed into perfectly healthy babies. PGD, in essence, might be throwing away valuable, viable embryos.
As many as half of all human embryos that have been examined in laboratories exhibit signs of mosaicism -- they are a patchwork of chromosomally normal and abnormal cells. And if the biopsied cell is abnormal, the embryo is rejected.
But there’s a new appreciation that such mosaic embryos may yield normal babies because the embryos can self-correct as they grow. Scott says his lab has taken embryos diagnosed as abnormal upon genetic testing and found that about one-third of them have self-corrected when tested again two days later.
One possible reason for such changes is that the PGD test is not 100% accurate. The standard aneuploidy-detection technique involves spreading the biopsied cell’s chromosomes on a slide, adding fluorescently tagged probes of different colors and counting colored dots. Sometimes, in this jumble of color, a chromosome is missed, or an extra one counted when it’s not there. Thus, good embryos could be tossed out.
But Scott, Behr, Racowsky and others also hypothesize that the aberrant cells within the embryo somehow get excluded or out-competed as embryonic development proceeds.
*
More harm than good?
Potentially more serious -- although also much more hypothetical -- is the issue of whether removing 12.5% of an embryo is truly harmless. Many fertility experts say they’re not sure. “We really do not know yet,” Racowsky says. “My view is that the less one perturbs an embryo, the better.”
What few studies there are suggest that rates of pregnancy after PGD are very similar to rates with normal IVF. But these studies, Racowsky says, are small and not definitive. “I would be very, very surprised if implantation rates overall were not compromised by the removal of a cell from the embryo,” she says.
There is also scant evidence that PGD impairs an embryo’s early growth or its ability to attach to the uterus. But although scientists have long thought that the cells of an early mammalian embryo are equivalent and therefore interchangeable -- identical twins, after all, derive from the splitting of a very early embryo -- some new data suggest that’s not so. Researchers now know that amounts of certain proteins and activity of certain genes differ among early embryonic cells, implying they are not exactly the same.
Other evidence comes from an attempt by a biotechnology company to produce embryonic stem cells from discarded IVF embryos. In that study, published last year, only a small percentage of the removed cells kept their ability to divide readily and become many different types of tissues. “In my opinion there was some destiny already predetermined in an eight-cell embryo that dictates what it becomes,” Behr says. Could removing one cell thus affect development of an embryo?
Only long-term follow-up will reveal whether subtle effects of PGD manifest years after a child is born, experts say. Although a national registry tracks the progress of pregnancies induced by IVF, no counterpart exists for PGD in the U.S. A tracking system for babies born after PGD is now in the works, says Susannah Baruch, director for reproductive genetics at the Genetics & Public Policy Center. The results won’t be known for some time.
Thus, for all of PGD’s prowess when used appropriately, fertility experts say that some caution may be in order.
“Assuming the biopsy is always benign is not smart,” Behr says. “I don’t think it is.”