Medical plans dangle gift cards and cash to get patients to take healthy steps
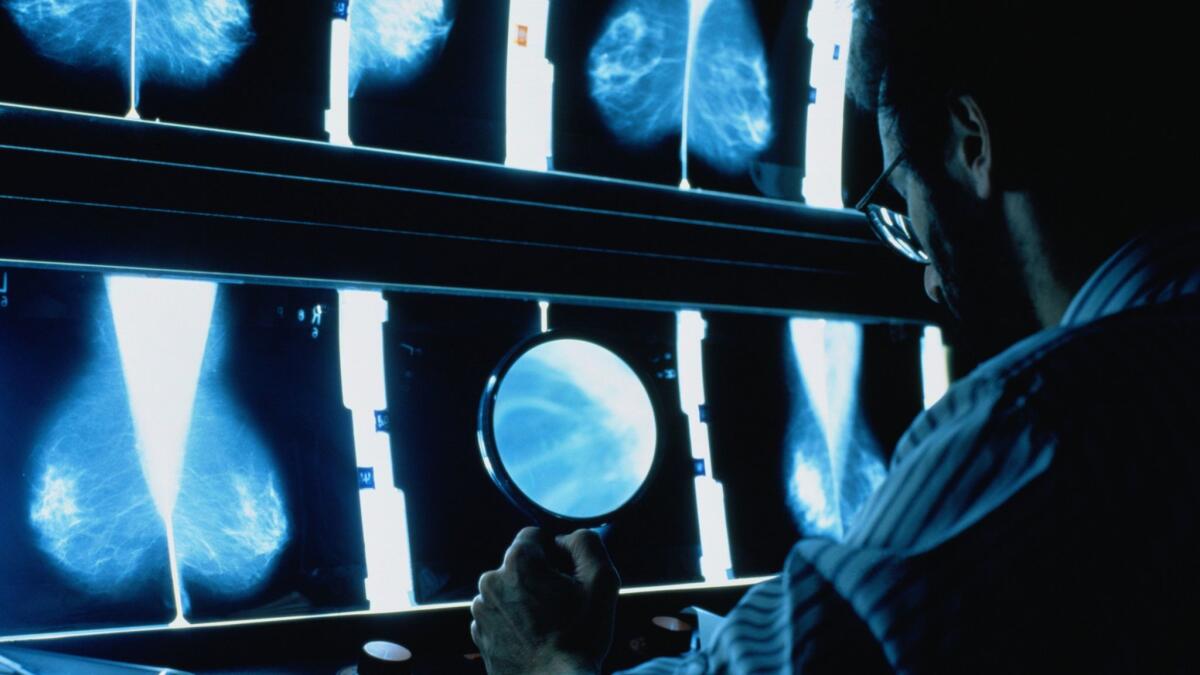
Patricia Alexander knew she needed a mammogram but just couldn’t find the time.
“Every time I made an appointment, something would come up,” said Alexander, 53, who lives in Moreno Valley.
Over the summer, her doctor’s office, part of Vantage Medical Group, promised her a $25 Target gift card if she got the exam. Alexander, who’s insured through Medi-Cal, California’s version of the Medicaid program for lower-income people, said that helped motivate her to make a new appointment — and keep it.
Health plans, medical practices and some Medicaid programs are increasingly offering financial incentives to motivate Medicaid patients to engage in more preventive care and make healthier lifestyle choices.
They are following the lead of private insurers and employers that have long rewarded people for healthy behavior such as quitting smoking or maintaining weight loss. Such changes in health-related behavior can lower the cost of care in the long run.
“We’ve seen incentive programs be quite popular in the insurance market, and now we are seeing those ramp up in the Medicaid space as well,” said Robert Saunders, research director at the Margolis Center for Health Policy at Duke University.
Medicaid patients who agree to be screened for cancer, attend health-related classes or complete health risk surveys can get gift cards, cash, gym memberships, pedometers or other rewards. They may also get discounts on their out-of-pocket health care costs or bonus benefits such as dental care.
Under the Affordable Care Act, 10 states received grants totaling $85 million to test the use of financial rewards as a way to reduce the risk of chronic disease among their Medicaid populations. During the five-year demonstration, states used the incentives to encourage people to enroll in diabetes prevention, weight management, smoking cessation and other preventive programs. The states participating were California, Connecticut, Hawaii, Minnesota, Montana, Nevada, New Hampshire, New York, Texas and Wisconsin.
Medi-Cal, for example, offered gift cards and nicotine replacement therapy to people who called the state’s smoking cessation line. Minnesota’s Medicaid program handed out cash to people who attended a diabetes prevention class and completed blood work.
An evaluation of these programs, released in April, showed that incentives help persuade Medicaid beneficiaries to take part in such preventive activities. Participants said gift cards and other rewards also helped them achieve their health goals. But the evaluators weren’t able to show that the programs prevented chronic disease or saved Medicaid money. That’s in part because those benefits could take years to manifest, according to the evaluation.
Overall, research on the effectiveness of financial incentives for the Medicaid population has been mixed. A report this year by the Center on Budget and Policy Priorities found that they can induce people to keep an appointment or attend a class but are less likely to yield long-term behavior changes, such as weight loss. And in some cases, the report said, incentives are given to people to get exams they would have gotten anyway.
The center’s report also found that penalties, including ones that limit coverage for people who don’t engage in healthful behaviors, were not effective. Instead, they can result in increased use of emergency rooms by restricting access to other forms of care, the report said.
Some of the biggest factors preventing Medicaid patients from adopting healthful behaviors are related not to medical care but to their circumstances, said Charlene Wong, a pediatrician and health policy researcher at Duke University.
That makes administering incentive programs more complicated. Even recruiting and enrolling participants has been a challenge for some states that received grants through the Affordable Care Act.
“The thing that is most likely to help Medicaid beneficiaries utilize care appropriately is actually just giving them access to that care — and that includes providing transportation and child care,” said Hannah Katch, one of the authors of the report by the Center on Budget and Policy Priorities. Another barrier is being able to take time off work to go to the doctor.
But health plans are eager to offer patients financial incentives because it can bring their quality scores up and attract more enrollees. And medical groups, which may receive fixed payments per patient, know they can reduce their costs — and increase their profits — if their patients are healthier.
Providing incentives to plans and medical groups has created a business opportunity for some companies.
Gift Card Partners has been selling gift cards to Medicaid health plans for about five years, said CEO Deb Merkin. She said health insurers that serve Medicaid patients want to improve their quality metrics, and they can do that by giving incentives and getting patients to the doctor.
“It is things like that that are so important to get them to do the right thing so that it saves money in the long run,” she said.
Agilon Health, based in Long Beach, runs incentive programs and other services for several California medical groups that care for Medi-Cal patients. The medical groups contract with the company, which provides gift cards to patients who get mammograms, cervical cancer exams or childhood immunizations. People with diabetes also receive gift cards if they get their eyes examined or blood sugar checked. And the company offers bonuses to doctors if their Medicaid patients embrace healthier behaviors.
The incentives for patients are “massively important for the Medicaid population, because the gaps in care are historically so prevalent,” said Ron Kuerbitz, CEO of Agilon. Those gaps are a big factor pushing up costs for Medicaid patients, because if they don’t get preventive services, they may be more likely to need costlier specialty care later, Kuerbitz said.
Emma Alcanter, who lives in Temecula, received a gift card from her doctor’s office after getting a mammogram late this summer. Alcanter, 56, had noticed a lump in her breast but waited about two years before getting it checked, despite reminders from her doctor’s office. “I was scared they were going to find cancer,” she said.
Alcanter finally decided to get screened after her first grandchild was born. The gift card was an added bonus, and Alcanter said it showed her doctors cared about her. Her mammogram revealed that the lump wasn’t cancer, and she plans to use the gift card to buy a present for her grandson.
Gorman is a senior correspondent for Kaiser Health News, an editorially independent publication of the Kaiser Family Foundation.
agorman@kff.org
Twitter: @AnnaGorman
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.






