This company made billions by surprise-billing helpless ER patients. Then justice arrived
- Share via
Some businesses deserve sympathy when they land in bankruptcy. Then there’s Envision.
The Tennessee company prospered as a provider of medical staff to hospitals around the country. It concentrated on emergency physicians, anesthesiologists and radiologists for a simple reason: Their patients typically had no ability to pick and choose among these doctors when they need care.
Waiting to be seen at the emergency room or already laid out on an operating table, the patients weren’t in a position to ask whether the doctor was in their insurance plan’s network.
These higher payment rates [are] caused not by supply or demand, but rather by the ability to “ambush” the patient.”
— Zack Cooper et al, Yale University
They might not even know they were seen by out-of-network doctors until they received a bill for their services — a surprise invoice for hundreds or even thousands of dollars.
Envision’s “secret sauce was to pile medical debt on people with emergencies,” says Eileen Appelbaum, co-director of the Center for Economic and Policy Research, a nonprofit Washington think tank. “That was purely taking advantage of people at their most vulnerable time.”
Get the latest from Michael Hiltzik
Commentary on economics and more from a Pulitzer Prize winner.
You may occasionally receive promotional content from the Los Angeles Times.
Envision stands as a case study in the destructive incursion of the profit motive — actually, the profiteering motive — in American healthcare.
Doctors themselves aren’t the problem — they’re disadvantaged themselves by financial pressures imposed by profit-seeking firms, which often require them to see more patients in a day and work without the best equipment.
Surprise billing — sometimes known as “balance billing” — by Envision and other firms like it elicited so much public outrage that Congress was finally moved to do something about the practice. In 2020 it enacted the No Surprises Act, which went into effect on Jan. 1, 2022.
Envision wasn’t alone in sticking patients with unexpected bills; another staffing firm, TeamHealth, is also struggling with the ramifications of the No Surprises Act.
The act prohibited out-of-network providers who were not chosen by a patient from charging the patient more than the in-network reimbursement fee set by the patient’s health plan. It forbade insurers to reject outright a patient’s claim for service from an out-of-network doctor.
Federal officials estimated that the law would apply to about 10 million unexpected bills a year. That figure didn’t include beneficiaries of another provision, which outlawed the very sleazy practice by some big insurers of rejecting an emergency-room claim because a patient’s condition didn’t turn out to be a true emergency.
The No Surprises Act blew a sizable hole in Envision’s profit-and-loss statement — part of “a whiplash-inducing onslaught of obstacles and complications” facing the firm’s management, its bankruptcy filing stated.
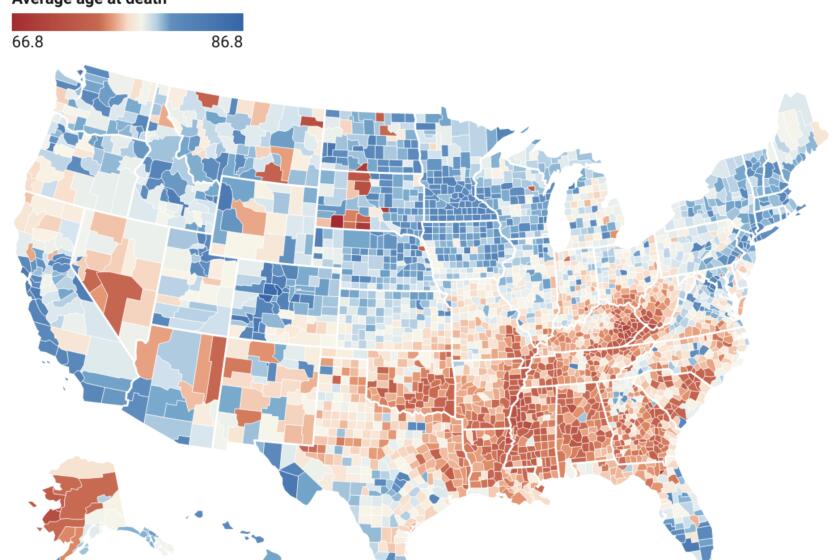
After decades of increasing longevity, Americans are facing shorter life spans than their predecessors and their rich-country peers. In states where Republicans set the agenda, it’s even worse.
Among other elements of the “onslaught” the firm cited was the COVID-19 pandemic, which reduced non-emergency hospital visits by as much as 70% because patients deferred elective surgeries; an increase in salaries for professionals as the pandemic prompted older clinicians to retire; and a billing backlash by its largest payer, UnitedHealth Group.
Envision, which provides staff for more than 500 facilities in 45 states, said in its bankruptcy filing that the pandemic cost it some $795 million in operating revenue (technically, earnings before interest, taxes, depreciation and amortization, or EBITDA) in 2020 and 2021.
UnitedHealth’s “uniquely aggressive” pushback on reimbursements, Envision said, cost it more than $400 million in EBITDA over the last five years. Envision says that if UnitedHealth merely paid what Envision claims it owes, it would not have had to file for bankruptcy. Overall, the company’s EBITDA went from about $1 billion before the pandemic to about $250 million last year.
In any case, the No Surprises Act was the factor that hit Envision’s business model below the water line.
It’s worthwhile, then, to take a closer look at what this firm and its owner, the private equity firm Kohlberg Kravis Roberts & Co., have been up to, and why we should celebrate the modest change in the American healthcare system represented by the act. (TeamHealth is owned by another private equity firm, Blackstone.)
Private equity firms acquire businesses typically through leveraged buyouts, in which the acquisition is financed largely through borrowings to be paid back out of the acquired business’ revenues. Generally, their goal is to cash out by selling the business or taking it public within about five years.
The firms first showed interest in healthcare businesses in the 1990s, initially focusing on nursing homes and hospitals because of their reliable cash flows, as a Brookings Institution study outlined in 2021. By 2010, the private equity firms had moved on to urgent care clinics, ambulance services, and emergency departments and hospital services such as anesthesiology and radiology “that could utilize surprise out-of-network billing,” Brookings found.
Eli Lilly’s price cuts on insulin will increase its profits, thanks to America’s bizarre drug pricing system. Don’t mistake its move for philanthropy.
According to a 2018 Yale University study that heavily influenced the legislative movement in Congress, it wasn’t unusual for emergency doctors to end their network contract with insurers. On average, the Yale researchers reported, out-of-network physicians charged more than twice the going in-network insurance reimbursements and more than six times the standard reimbursements from Medicare.
The study in effect pointed the finger at the physician staffing firms, Envision (known at the time as EmHealth) and TeamHealth. “Both firms profit from the fact that out-of-network physicians working in in-network hospitals cannot be avoided by patients.” The runup in charges, the researchers wrote, “undercuts the functioning of healthcare labor markets, exposes patients to significant financial risk, and reduces social welfare.”
“These higher payment rates” charged by out-of-network physicians, the Yale study said, are “caused not by supply or demand, but rather by the ability to ‘ambush’ the patient.” The practice raised the cost of healthcare generally.
The Yale researchers made passing mention of another player in this process: the health insurance industry, which has an interest in paying providers as little as it can get away with. (UnitedHealth, as it happens, provided the researchers with the data they used for their study, leading to accusations that the study favored the health plans’ point of view; the researchers said UnitedHealth had no influence on their findings.)
Insurers reacted to the charges from out-of-network doctors by paying only a portion of their bills. That prompted doctors to try to obtain the balance by billing the patients. The surprise billing scandal was born.
Envision says it started to phase out surprise or balance billing in 2020, even before the No Surprises Act was passed and signed — though congressional action against the practice was in the wind long before that.
It says its real problem is that regulations implementing the act have put health insurers in the driver’s seat in setting reimbursements. Provider firms have to go to arbitration to settle their differences, but that’s resulted in a logjam of arbitration cases and a backup of unpaid claims.
Private equity investors had long had their eyes on Envision, which was founded in 1992. The firm oscillated between private and public ownership, as a succession of investors sought to squeeze it for profits.
The process started in 2005, when Onyx Capital acquired it through a leveraged buyout and took it public the same year. The investment firm Clayton, Dubilier & Rice acquired it in 2011 for $3.2 billion and staged an initial public offering two years later.
Soon after that, EmHealth merged with Amsurg, a physician staffing service for ambulatory surgical centers — that is, those unaffiliated with hospitals. The result was Envision, which became the largest physician staffing firm in the country.
Moderna and Pfizer have announced plans to quadruple the price of their COVID vaccines, putting them out of reach for millions. The U.S. should step in.
Kohlberg Kravis Roberts entered the scene in 2018 with a $9.9-billion leveraged buyout, in which the firm and its partners invested $3.5 billion. That stake was wiped out in the bankruptcy, which followed lengthy and extremely complex negotiations with creditors that included Newport Beach-based Pimco.
The prearranged bankruptcy will allow both Amsurg and Envision to continue operating under the ownership of their creditors, who will take over once the latter emerges from bankruptcy in the fall. Among the new owners will be Blackstone, giving the big private equity firm a foothold in the two biggest staffing companies, Envision and TeamHealth.
The No Surprises Act did little to remedy the dysfunction of American healthcare. If anything, it underscored the insanity of a system that locks providers and payers in never-ending conflict over who owes what to whom and for which services.
Envision and UnitedHealth waged this war for years. The two parties let their last network contract expire in January 2021, after which they continued to snipe at each other over reimbursements until last September, when they served each other with lawsuits.
Envision says UnitedHealth has consistently low-balled its reimbursements ever since the contract expiration — in fact, it says Envision allowed the contract to lapse because it wouldn’t accept UnitedHealth’s “unconscionable take-it-or-leave-it reimbursement offer.”
The insurer, for its part, says Envision has “systematically” upcoded its reimbursement claims. The allegation is that Envision has submitted claims for more elaborate patient treatments — which warrant higher reimbursements — than the patients needed or received at the ER.
(Envision won a $91-million arbitration award from UnitedHealth in March, but that dispute concerned reimbursements owed in 2017 and 2018, while the firms’ network contract was in effect.)
It’s tempting to declare a plague on both their houses, to quote “Romeo and Juliet,” but the problem is systemic. It’s grounded in “the tension between profit maximization by firms that own healthcare providers, and the best care possible for patients that providers are obligated to provide,” Appelbaum has observed.
The No Surprises Act addressed one symptom of that tension, the practice of sticking unwary patients with unexpected bills. But it didn’t lay a finger on the underlying disease. Americans spend vastly more on medical care than residents of any other developed country, and have worse health outcomes.
One reason is the endless, costly dickering among middlemen like Envision and UnitedHealth to make sure they get their share of the bucks sloshing around in the system. Every segment of the healthcare industry also spends heavily on lobbyists in Washington to ensure they don’t get shut out of the party.
Who doesn’t have lobbyists? The patients. The No Surprises Act is one of the very few victories they’ve ever notched in this battle, and they shouldn’t expect to see many more.
More to Read
Get the latest from Michael Hiltzik
Commentary on economics and more from a Pulitzer Prize winner.
You may occasionally receive promotional content from the Los Angeles Times.