
- Share via
Lisa Dabby sees fear in the patient’s eyes. They are wide and bugged out. The pupils are haloed in white.
Brow beaded with sweat, the patient sits in street clothes, alone on a plastic chair in a tent set up in a driveway, a makeshift emergency room.
Dabby takes her stethoscope and hears a crackle inside the lungs.
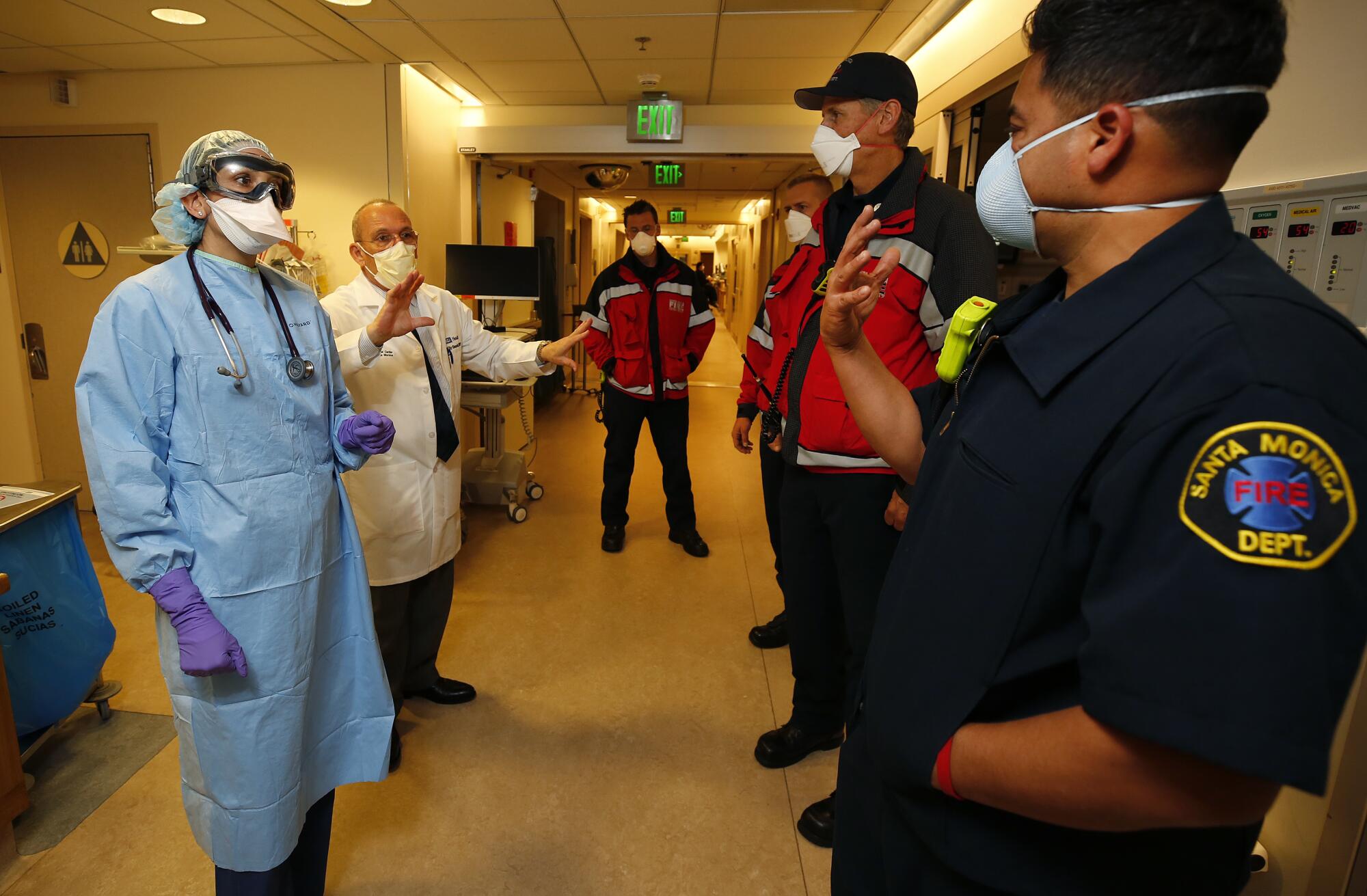
She is a doctor in the ER at UCLA Medical Center in Santa Monica. She treats patients who might otherwise die from unexpected trauma and illness.
This patient is drowning in open air.
A nurse has taken a history — fever, body ache, cough — so Dabby asks simple questions requiring nothing more taxing than a nod or a shake of the head. She promises tests, a bed, oxygen and wishes she could do more.
Like everyone, she listens to politicians and public health officials debate when to reopen the country. Each morning she looks at the numbers and is encouraged: The curve seems to be flattening.
But still she worries.
“People keep referring to us as the front line,” she says later over the phone. “We’re not the front line. Every individual in our country is the front line. All the coronavirus wants to do is spread, and everyone needs to realize they have the power to stop it.”
The patient drowning in lung fluid weighs on her mind.
It is an evening shift in April, and in subsequent phone interviews she vividly recalls the events of this night. The patient arrives at the hospital and is directed to the COVID-19 screening tent. The terror Dabby sees in the eyes is the terror she sees in the most severe cases.
She finishes her exam, steps outside the tent, unsnaps her gown, removes her gloves and uses sanitizer. The alcohol stings her dry, cracked hands.

She looks at the patient’s X-ray.
“Ohh,” she sighs, and catches herself.
Whitish-gray patches cloud the far reaches of the lungs, where the picture is normally black.
Ground-glass opacities, she thinks, repeating a textbook description, the classic presentation of multi-focal pneumonia and COVID-19.
A nurse helps the patient to a room inside the hospital.
Dabby hasn’t lost anyone to COVID-19, although three patients are on ventilators upstairs.
For weeks, staff at the hospital had waited for an anticipated wave of cases that never arrived, but each day brings a steady stream, which might be manageable if the disease itself were manageable.
‘I have nobody, no family, and I am just really scared to die alone.’
— COVID-19 patient
Without a cure or treatment, however, the playbook is always changing.
“It is frustrating, unsettling — I don’t have the right adjective for it,” she says. “For the first time in my life, I don’t know what will work. I’ve been asked to treat an illness without the answers.”
::
She recalls another patient sobbing with fear.
Dabby is returning from the Personal Protective Equipment room with clean goggles, a new face mask, fresh gloves and an unsoiled gown, double checked that all the buttons are snapped.
She sees this patient sitting by herself and disconsolate. “I have nobody, no family,” the patient says, “and I am just really scared to die alone.”
Dabby takes a nearby chair. Patients can’t read expressions through protective garb, so Dabby reaches out and cups the patient’s open hand in her own.
Through purple medical gloves, Dabby feels warmth. Isolation and illness are a terrible combination, and her words come easily.
“We’re very good at screening,” she says, “and there is nothing dangerous happening right now with your heart and lungs. Your oxygen level looks good.”
The patient nods.
“We’ll get an X-ray, an EKG and send a swab out for COVID testing.”

Dabby doesn’t see a need to expedite the test, but she will call a social worker to sit with the patient.
“I feel thoroughly sad for the world right now,” Dabby says over the phone. She is calling from her home in Brentwood where she lives with her husband and three children.
“This is a lonely time for people who live alone.”
She says she used to sleep easily, eight hours at a stretch, but now she needs Benadryl to help.
Early in the pandemic, she kept waking at 4 a.m. with her heart racing. She got up, made tea and started reading posts from other doctors, various journals, anything that might help her with her patients.
She concedes: The pace is wearing her out.
::
Other patients stand out in her mind.
Two came to the ER in March, just hours apart from one another. They were young — late 30s, early 50s — and she wouldn’t have given them a second thought if she had passed them on the street.
They made her realize that some of her assumptions about this pandemic — afflicting mostly older people, those with co-morbidities — have exceptions, and she doesn’t know what to do.
She never likes feeling helpless. It reminds her of why she became a doctor, the feeling during childhood of watching her grandparents die two years apart and being unable to do anything.
She knows what to do about heart attacks, strokes, sepsis, internal bleeding, respiratory distress, but now she struggles for answers.
Dabby also recalls another earlier case: a young woman, pregnant with twins, due in a week, who tested positive for COVID-19 and wanted to know if she would be able to hold her babies.
Could she breastfeed them? Could her husband join her in the delivery room?
Dabby didn’t know.
That uncertainty hovers over everything in the ER, even for one of the cases this night, an apparent overdose. This patient is a rag doll, barely breathing, and like everyone who comes into the emergency room, is treated as if infected with the coronavirus.
Dabby watches as nurses move in with a hand-held respiratory bag, something they have done countless times.
“Wait!” Dabby calls out.
Their first reflex — care in a matter of seconds — has betrayed them. They are not wearing their PPEs. Each day brings changes to the most ordinary procedures. Workflow and safety are constantly reassessed.
For the overdose patient — who may or may not have COVID-19 — time is running out.
Fully dressed in PPEs, the nurses squeeze and relax the respiratory bag. They administer medication to block the effects of a possible opioid.
But nothing works.
Breathing slows. Eyes are shut. The patient is nonverbal, not moving.
Dabby decides to intubate.
Because of COVID-19, intubation is now one of the riskiest procedures in the emergency room.
Early studies suggested that the coronavirus was transmitted through droplets, conversational spittle falling to the ground no farther than six feet away. Today experts believe it can be passed in aerosol form, the mist of the breath hanging in the air and filling a room.
Intubation increases exposure to droplets and aerosol.
A technician helps Dabby into a new set of PPEs and a face shield fitted with a special respirator to keep her safe from airborne pathogens.

Seconds feel like minutes as she watches the patient decline.
Dabby asks a nurse to add anesthesia and a paralyzing drug to the patient’s IV. Dabby guides a laryngoscope between the tongue and the epiglottis. The vocal cords come into view, two pearly strands.
A tracheal tube follows, and a respiratory therapist switches on a ventilator.
The patient is taken to the intensive care unit, and a near-lethal combination of opiates, alcohol and marijuana is eventually metabolized.
The COVID-19 test comes back negative.
One of her last patients before the end of her shift is a surgeon with fever, body aches, cough and the distress of having contracted the virus.
Dabby takes a swab and promises expedited handling. “Let’s take it one step at a time,” she advises. “Stay at home until you get the results.”
She thinks about her own vulnerability and what she might bring home. Some doctors are staying in hotels, but her husband doesn’t want her to move out.
So she set rules: no sharing food or the same bathroom, no hugging, no kissing.
“I feel like there is a struggle between my commitment as a professional and my responsibility to my family,” she says on the phone. “That is what is really scary. It is one thing for me to be in harm’s way, but it is not fair to my family.”
::
Before going home, she changes her clothes and puts her scrubs in a bag. She wipes down her stethoscope, pen, phone, glasses and identification badge.
In her garage, she drops the bag of scrubs on the floor, where it sits for a week, time for the virus to die.
Inside her home, her husband and young children are asleep. This is her loneliest hour.
She showers, washes her hair and scrubs her skin.
She goes to a room away from her family and climbs into bed. In her mind, she sees the patient who was drowning in open air, eyes wide with fear.
After three weeks on a ventilator, the patient is now on dialysis. In addition to the lungs, COVID-19 can attack the kidneys.
The patient is breathing without help, but still fighting for life.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.










