Smaller doses of monkeypox vaccine got the OK. Here’s how that works at one clinic

Mark Webber and Doug Brown rose before dawn to make the trip from Agoura Hills, arriving around 6 a.m. at the Leimert Park clinic in the hopes of getting vaccinated against monkeypox.
“We came out in the ‘80s. We remember when HIV blew through,” said Webber, 54, a Maryland resident who has been in Southern California to care for his late father. As monkeypox has arisen as a health threat, “we take it very seriously.”
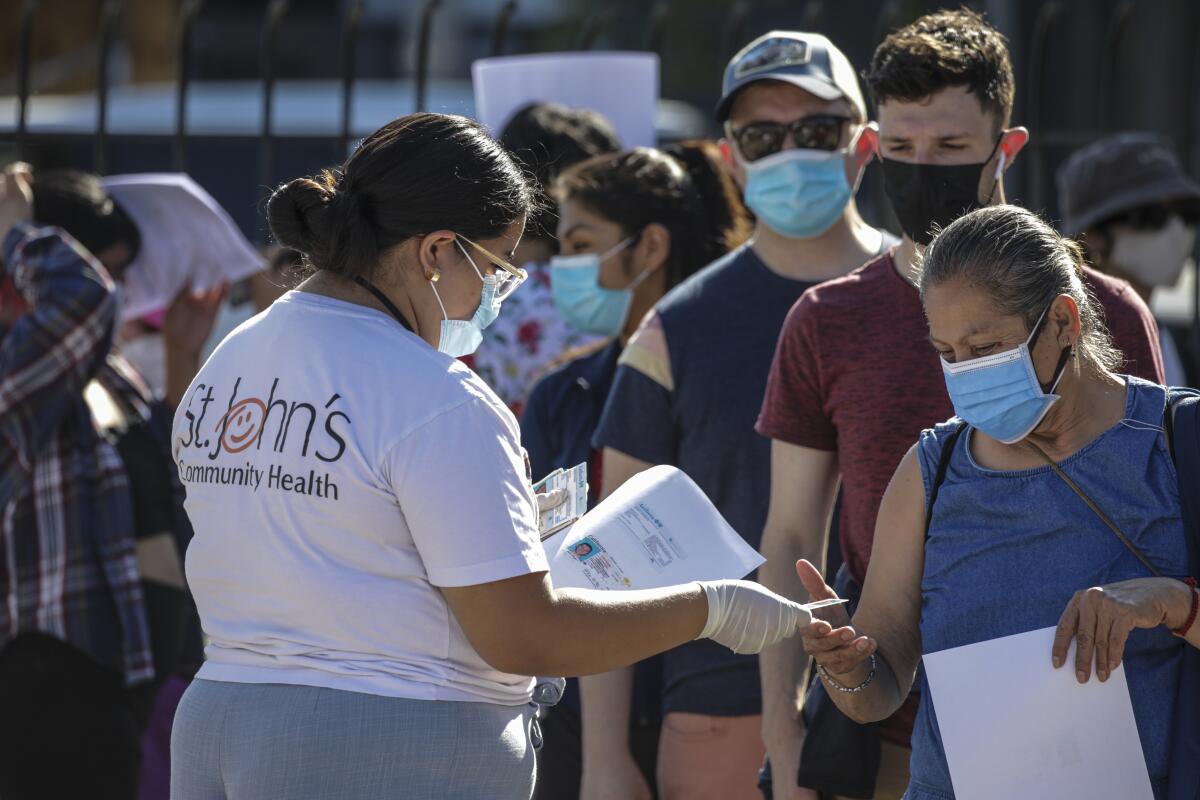
The line began to form hours before the Crenshaw Boulevard clinic began administering shots Wednesday, snaking through the parking lot of the St. John’s Community Health site. Inside the clinic, health workers had split each vial of Jynneos vaccine into five doses, after federal officials gave the green light Tuesday to change the way the shots are administered.
In the broiling heat, St. John’s nursing director Gale Castillo walked down the line of patients awaiting their shots, explaining what to expect: The vaccine would not be given subcutaneously — in the fatty tissue under the skin — but at a shallower level in the skin. “If you’ve ever had a TB test? Same thing,” Castillo told them, displaying photos of the process.
The Jynneos vaccine, a shot approved by the Food and Drug Administration to protect against monkeypox, has been in limited supply as Angelenos try to avoid the virus. The infectious disease is rarely fatal, but can cause fevers, aches, swollen lymph nodes and painful lesions, and has forced people to isolate themselves for weeks.

As demand has outstripped supply, Los Angeles County has limited who is eligible for the vaccine, only offering the shots to people deemed to be at higher risk. It has also been urging health providers to prioritize giving out first doses of the Jynneos vaccine — meant to be provided in two doses at least four weeks apart — over ensuring that people get their second dose.
Federal officials also announced Tuesday that they would stretch the monkeypox vaccine supply by allowing medical providers to give smaller doses at a shallower level in the skin. The method, called intradermal injection, has been previously used with other inoculations in short supply. The FDA cited a clinical study that found the smaller, shallower doses generated a similar kind of immune response as subcutaneous injections. Doing so could effectively quintuple the number of available shots, since the method uses only a fifth of a full dose.
“I think that this is a very smart utilization of the vaccine,” said Anne Rimoin, a professor of epidemiology at the UCLA Fielding School of Public Health. Rimoin said the plan was rooted in sound science, “but we will need to do some work to assess how effective it’s going to be.”
CDC director Dr. Rochelle Walensky told reporters Tuesday that the intradermal method was a better way of expanding vaccine access than only giving people a single shot. Dr. Rita Singhal, chief medical officer for the L.A. County public health department, said Thursday that it would “be opening up for second doses as we transition to the intradermal or alternate regimen.”
“We feel pretty strongly that the two doses are necessary, in part because we simply don’t have any evidence out ... months later after a single dose to know that people will be adequately protected,” said Dr. Peter Marks, director of the Center for Biologics Evaluation and Research at the FDA. “And we don’t want to give people a false sense of security.”
Although the shifting strategy around the vaccine has raised questions and concerns, the deputy coordinator of the White House monkeypox response said that the group hit hardest by the virus so far — men who have sex with men — has generally shown confidence in getting immunized, with COVID vaccination rates “well over 90%.”
For monkeypox, “we will likely still run out of vaccines before we run out of arms,” Dr. Demetre Daskalakis said.

The change was welcomed at St. John’s Community Health, which had already scheduled a vaccination clinic for the day after the shift in immunization strategy was announced. Dr. Anitha Mullangi, chief medical officer at the nonprofit healthcare provider, said its team had quickly mobilized to make the switch. One key change was that it would give the intradermal vaccinations on the underside of the lower arm, where it was easier to place the injection in the skin.
Ernesto Barahona, the chief development officer at St. John’s, said splitting the doses meant they now had enough for 1,800 patients in hand. The demand was plain in the August heat, with scores of people lined up outside. West Adams resident Ruben Ramirez, who encountered the line coiling through the parking lot when he arrived at 9 a.m., said he was undaunted.
“The wait doesn’t matter. It’s important,” Ramirez, a 59-year-old antiques dealer, said in Spanish. Ramirez didn’t want to get sick, but “my bigger concern is infecting other people.”
The rising number of monkeypox cases had fueled anxiety for Taylor Tobias, a 42-year-old actor who came to the clinic from West Hollywood. “What do I do if I’m covered in sores and I can’t work?” Tobias asked. At one point, “I went down a TikTok wormhole which really freaked me out.”
When Tobias gets the vaccine, “I’ll still take the same precautions” as now, the actor said. “But it does relieve some of the anxiety.”
Derek Catao had seen on the news that the federal government was changing the way the vaccine could be administered.
“I’m in favor of it if more people are protected,” said Catao, 47, who went to the vaccination clinic from Glendale. As cases have risen, “I fear it’s going to get worse before it gets better.”
Health officials say the virus is most commonly spread by skin-to-skin contact with contagious lesions, typically in intimate settings, although it is also possible for it be transmitted through contaminated sheets and respiratory droplets if there is extended exposure.
So far, the virus has disproportionately affected gay and bisexual men: In Los Angeles County, the overwhelming majority of cases reported so far have been among men, the bulk of whom identify as gay, bisexual or queer, according to county data.
Many gay and bisexual men have been putting off social and sexual activity or finding other ways to reduce their risks until they can get vaccinated, but “the vaccine is the definitive solution to this,” said Dr. Timothy M. Hall, health sciences assistant clinical professor at UCLA’s Center for Behavioral and Addiction Medicine.
Hall lamented that different expectations have been applied to gay men than straight people: “There’s this idea that gay men should be able to just turn off their sexual lives, their romantic lives, their relationships for an indefinite period of time.”
Although the virus has hit the gay community hardest, health and community groups have reiterated that the disease can affect anyone. Octavio Hardouin, a 35-year-old waiting in line Wednesday for the vaccine, said that “everyone needs to be aware of this virus.”
“This virus is not just for gay people,” Hardouin said. “Everyone can get it.”
As of this week, Los Angeles County had received more than 43,000 full doses of the Jynneos vaccine and administered more than 31,000 of them. Singhal, chief medical officer for the county public health department, said that with an upcoming shipment of additional doses and the increased capacity from the intradermal injections, L.A. County would be able to fully vaccinate 85,000 to 90,000 people — about half of what it believes to be the population now at risk.
Among those now eligible are gay and bisexual men and transgender people who had multiple or anonymous sexual partners in the last two weeks or are taking preventative medicine to avoid HIV, as well as other targeted groups.

St. John’s officials said their clinics require patients to fill out screening questions on an attestation form to determine their eligibility for the vaccine. By midday, when the morning line had evaporated, Barahona said that more than 200 people had gotten vaccinated; by the end of the day, the number exceeded 300, according to a St. John’s spokesperson.
The clinic had sent out text messages to patients about the vaccination event, but had also posted on Instagram and Facebook, where Webber learned about it. He and Brown were eager to get the vaccine after struggling to secure appointments for the shots at home in Maryland.
Like Webber, Brown invoked his memories of the beginnings of the AIDS crisis as he talked about wanting to protect himself against monkeypox. The 58-year-old recounted burying one of his friends who lost his life to AIDS. Monkeypox is rarely fatal, but Brown still saw resonance in that history.
“Everyone says it’s not a big deal,” Brown said, “until it’s a big deal.”
AIDS has also been on the mind of Jim Mangia, president and chief executive of St. John’s Community Health, as he sees gay men and others confront monkeypox as a health threat.
In the early days of the AIDS epidemic, “I was going to a funeral every other week. All my friends were dying,” said Mangia, who is gay. “The LGBT community came together and developed its own response, from messaging to support services to a whole host of prevention strategies.”
Now “the community needs to come together again to get those messages out — that this can be prevented,” Mangia said. “We just need a couple more weeks until we get ample vaccine.”
Times staff writer Rong-Gong Lin II contributed to this report.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.







