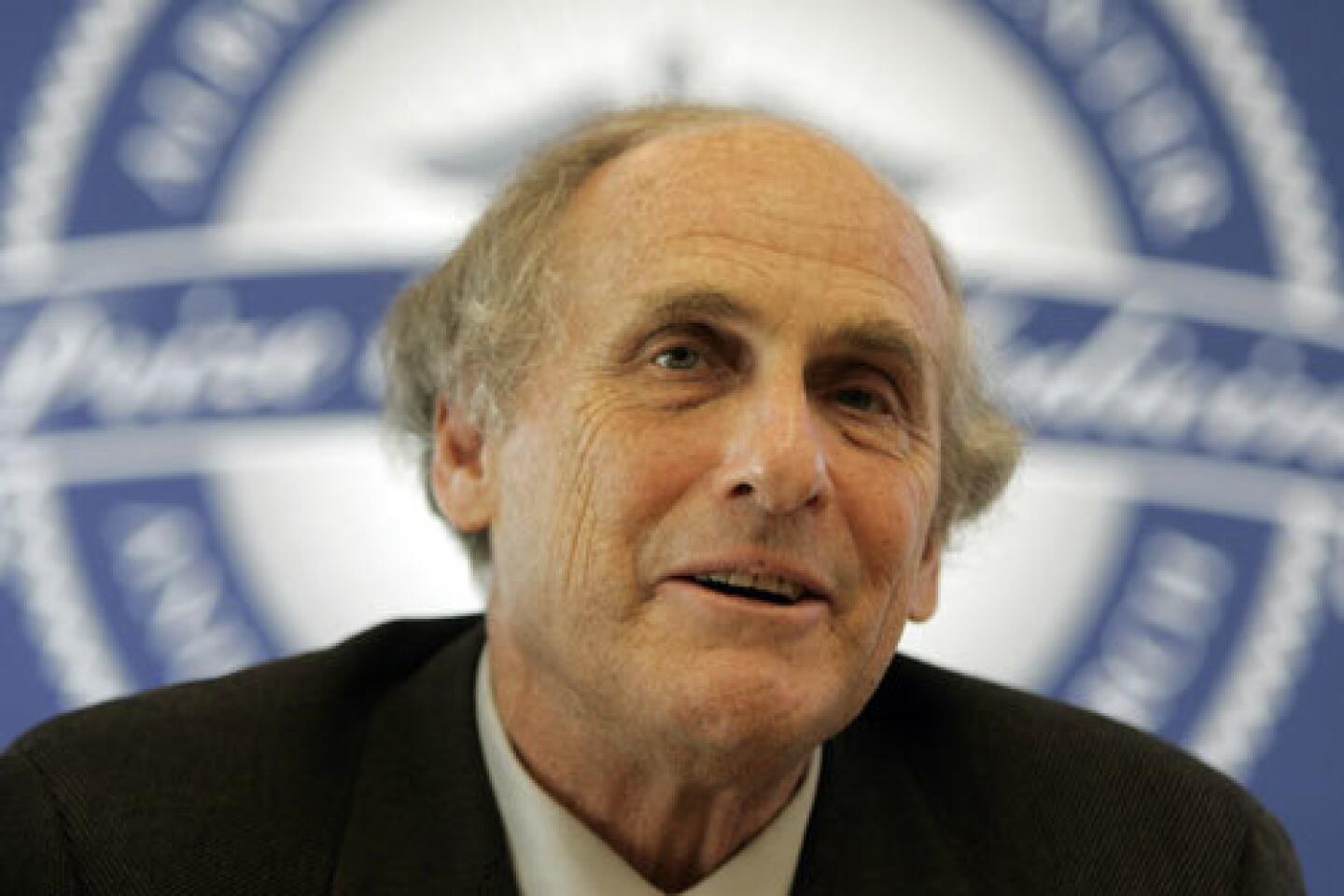
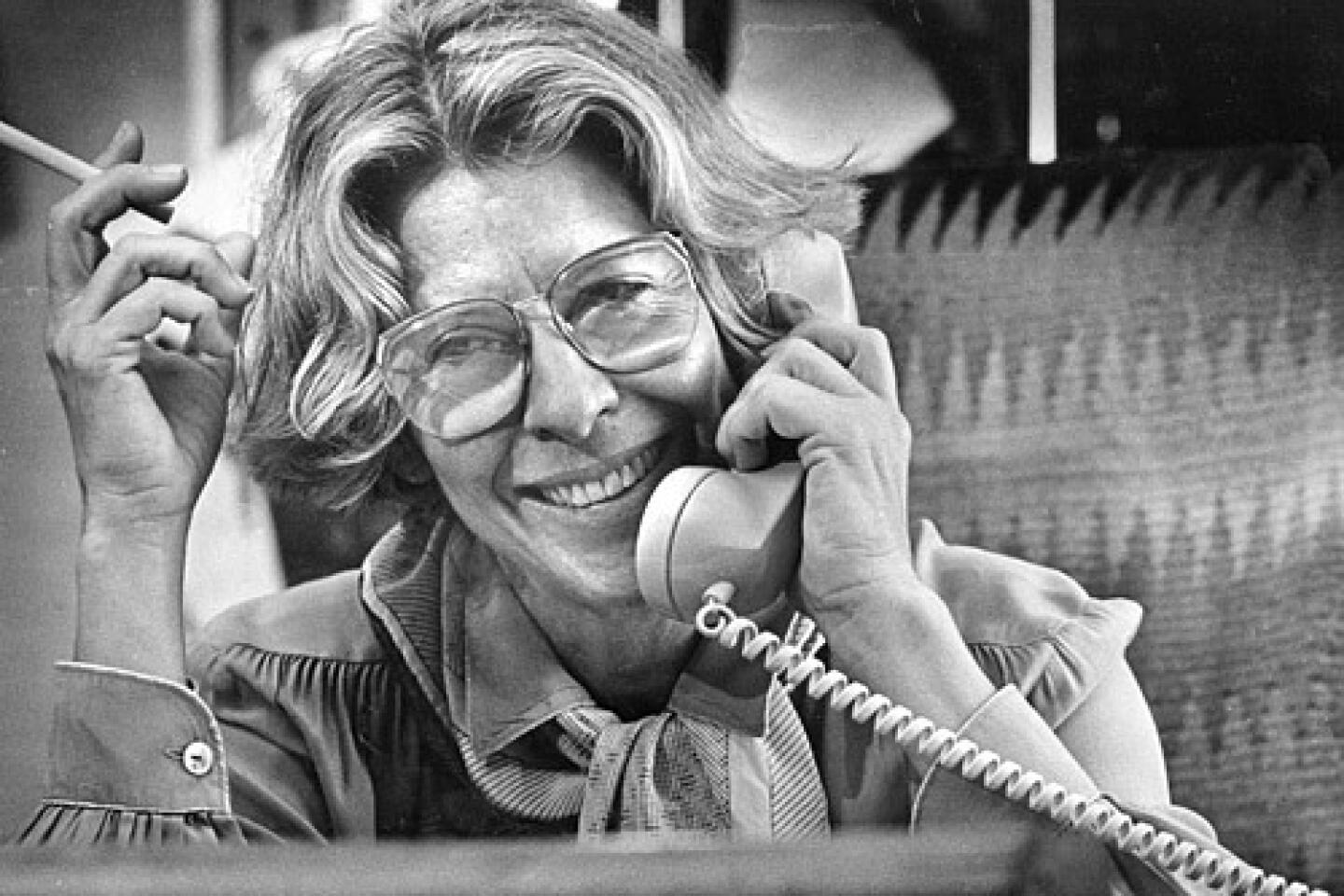
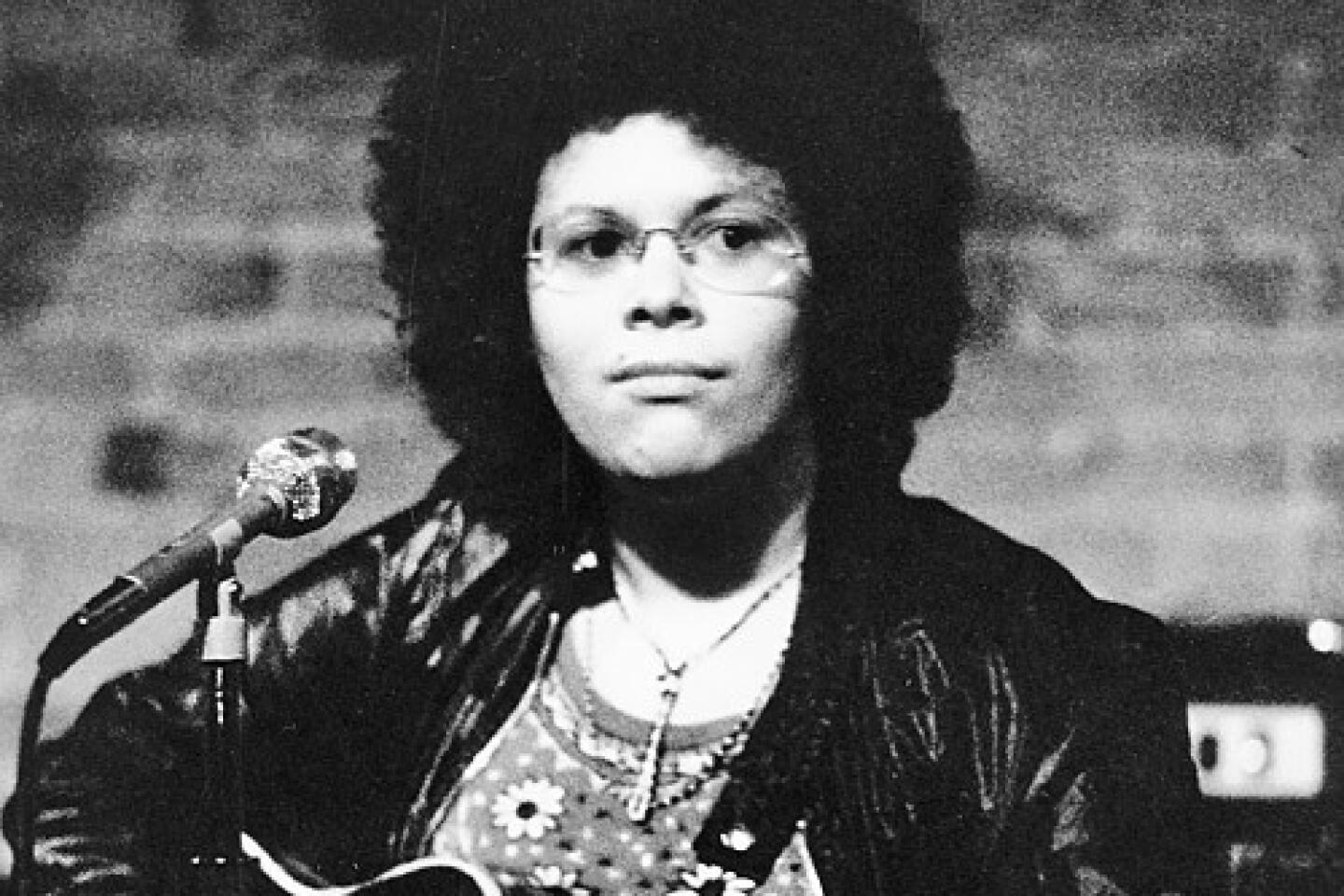
Rosalyn Yalow dies at 89; Nobel winner helped revolutionize medical diagnostics
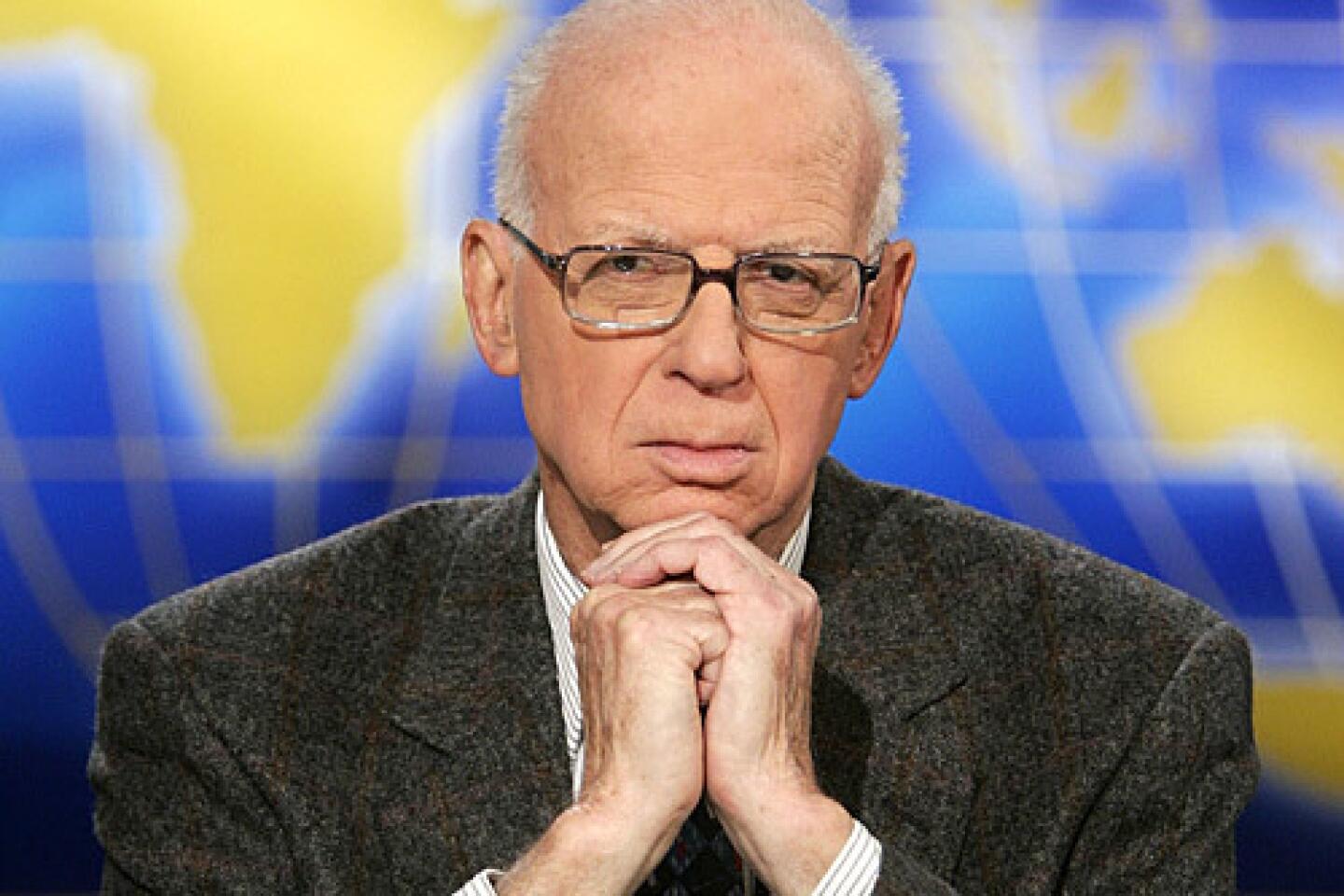
Physicist Rosalyn S. Yalow, who shared the 1977 Nobel Prize in Physiology or Medicine for the development of a medical diagnostic test that revolutionized patient care and led to a new understanding of diabetes and a host of other diseases, died May 30 in the Bronx, N.Y. She was 89. No cause of death was announced.
Although her work in medical diagnostics was seminal, she was perhaps equally well known for her temerity in entering a field that had previously been dominated by men and for her persistence in pursuing her goals in the face of opposition from the establishment and the opposite sex.
She was only the second woman to win the Nobel in medicine and only the sixth to win a Nobel in any science.
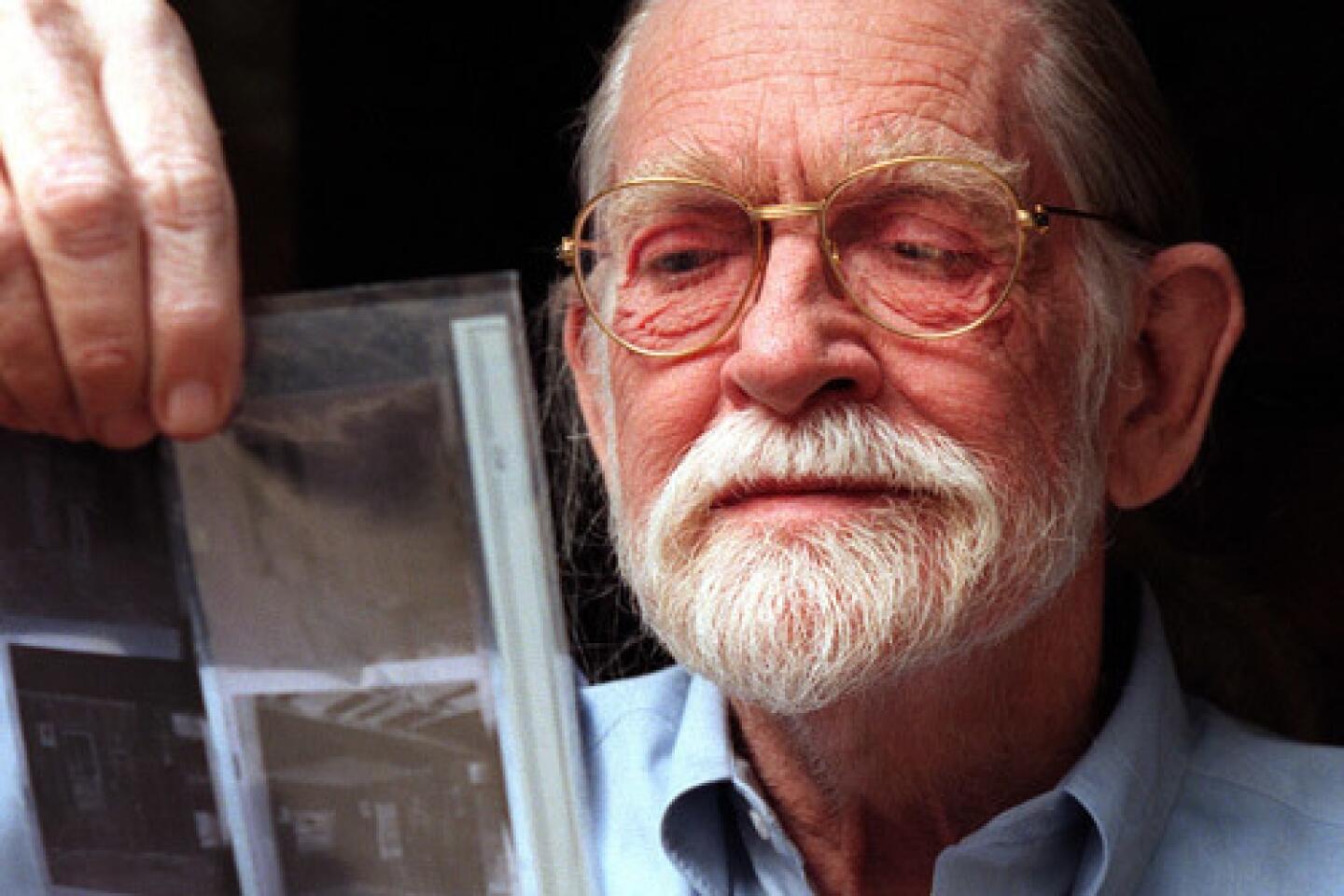
When Yalow and her colleague Dr. Solomon Berson began their research at the Bronx VA Hospital in the early 1950s, most medical diagnostics — which involve measuring the concentrations of hormones, vitamins and other biological molecules in the blood — was performed by strictly chemical techniques.
Such techniques were cumbersome and insensitive, particularly for measuring substances present in minute concentrations. A chemical assay for adrenocorticotropic hormone or ACTH, which is produced by the pituitary gland to stimulate the production of steroid hormones, required 250 milliliters of blood, or a little over a cup — too much to remove from a sick individual.
Yalow and Berson were in the VA hospital’s new radioisotopes laboratory, which was investigating the application of such isotopes for medical purposes, such as treatment of cancer. They had been working on a way to use the atoms to monitor blood volume.
The genesis of their Nobel experiments occurred when the pair observed that insulin injected into the bloodstream of patients persisted there longer when the patients had previously been exposed to the hormone, such as for treatment of shock or what was then called adult-onset diabetes.
They reasoned that the initial exposure to extrinsic insulin led to the production of antibodies against the hormone, and that these antibodies bound to the hormone and held it in circulation longer than it would have persisted otherwise. Such a conclusion, however, was tantamount to heresy because the prevailing wisdom was that antibodies could form against only relatively large foreign objects, like viruses and bacteria.
Peptide hormones, such as insulin, were simply too small to generate an antibody response, the conventional wisdom held. Peptides are strings of amino acids, much smaller than proteins.
Undaunted, the pair pressed ahead to develop an assay for insulin. First they prepared antibodies against insulin in animals, then attached the antibodies to a solid substrate, such as plastic beads, that would hold them in place. Next, they attached a radioactive isotope such as iodine-131 to free insulin and allowed this so-called hot insulin to occupy all the binding sites on the antibodies.
When blood containing even small amounts of insulin was then placed in a test tube with the beads holding the antibodies, unlabeled insulin in the blood — called cold insulin — would attempt to bind to the antibody, displacing some of the hot insulin.
When all the blood was washed away thoroughly, the researchers measured the radioactivity remaining on the beads. The less radioactivity on the beads, the more cold insulin that had been present in the blood sample. The test, which came to be called radioimmunoassay or RIA, proved to be very sensitive, making it possible to measure very small quantities of peptide hormones.
But when they attempted to publish their findings in 1956, their paper was rejected by both the journal Science and the Journal of Clinical Investigation because it contradicted the prevailing wisdom. Ultimately, the latter journal published the paper, but only after the authors had removed all references to antibodies. Yalow often showed that rejection letter in her later talks, including her Nobel acceptance speech.
In a subsequent series of papers throughout the rest of the decade, the pair described RIA in detail. The Nobel committee described their work as “a spectacular combination of immunology, isotope research, mathematics and physics.” RIA proved to be so sensitive that it could detect insulin in amounts as small as 10 picograms (10 thousand-billionths of a gram) per liter and ACTH in an amount less than 1 picogram.
In their follow-up work, the VA researchers created RIA tests for a variety of other hormones, vitamins, drugs, bacteria, viruses such as hepatitis B and other natural products. Their assay for the hepatitis virus allowed blood banks to screen for it for the first time, sharply reducing transmission via transfusions.
They were also able to use the tests to elucidate the physiology of the hormones insulin, ACTH and growth hormone and to shed light on diseases caused by abnormal production of the hormones.
They showed, for example, that adult-onset diabetes, now known as Type 2 diabetes, is caused not by lack of insulin secretion by the pancreas — the cause of Type 1 diabetes — but by increased resistance to the effects of insulin by tissues throughout the body. This moved diabetes research in an entirely new direction as researchers began looking for drugs that increased insulin sensitivity of tissues.
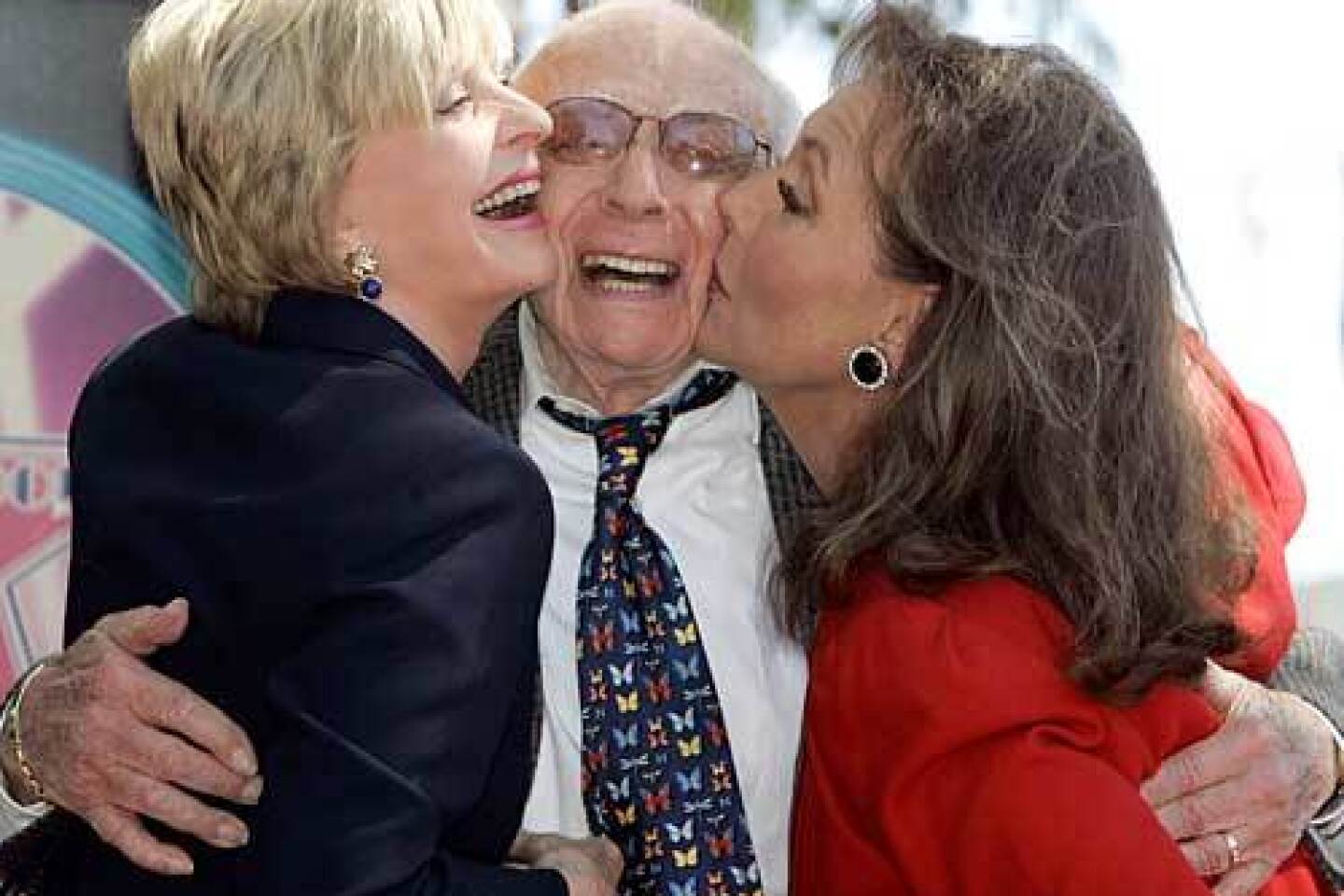
Berson died in 1972, before the Nobel committee considered their discoveries. Because the Nobel is never awarded posthumously, Yalow received half the award for her work. Roger Guillemin and Andrew Schally received the other half of the prize for their separate work on peptide hormones.
The Nobel citation noted that Yalow and Berson’s research was “pioneering work at the highest level. It had an enormous impact. We were witnessing the birth of a new era in endocrinology, one that started with Yalow.”
RIA has subsequently been displaced by related tests that use chemiluminescent or color-generating molecules as reporter molecules instead of radioisotopes.
Rosalyn Sussman was born in the South Bronx on July 19, 1921, the daughter of parents who never finished high school. But she was imbued with a love of reading, and her older brother Alexander took her to the library every week to get a fresh load of books.
In high school she developed an interest in chemistry, but after enrolling at Hunter College, now part of the City University of New York, her fascination switched to physics. In the 1930s, she later wrote, “physics, and in particular nuclear physics, was the most exciting field in the world.” She was also inspired by Eve Curie’s newly released biography of her mother, Marie Curie.
Upon her graduation, her parents thought she should become an elementary school teacher, but she had a higher aspiration: a graduate degree in physics. But universities were not equally enthusiastic. One Midwestern school wrote her advisor a rejection that noted, “She is from New York. She is Jewish. She is a woman.”
Ultimately, the shortage of male students engendered by World War II led to her receiving a graduate fellowship at the University of Illinois. When she arrived she found that she was the only woman on the College of Engineering’s faculty and staff of 400. “I was told I was the first woman there since 1917.”
Her grades were excellent, marred only by an A minus in a physics laboratory. The chairman of the physics department could only say, “That A minus confirms that women do not do well at laboratory work.”
On her first day in graduate school she met Aaron Yalow, who became her husband in 1943. He died in 1992.
Receiving her doctorate in nuclear physics in 1945, she joined the staff back at Hunter College, where she spent three years teaching. But research called to her, and in 1947 she took a part-time position at the Bronx VA, converting to full time a year later. She spent the rest of her career there.
Yalow is survived by a son, Benjamin, of the Bronx; a daughter, Elanna Yalow of Larkspur, Calif.; and two grandchildren.