How to prepare for the second pandemic — of mental health issues
- Share via
When she was in her late 70s, my late grandmother Henrietta became an unofficial mental health provider. Often housebound because of physical ailments, Grandma needed a volunteer effort she could do from her living room, so she became involved with the Jewish Family Services agency, calling half a dozen seniors every week.
The people she was assigned needed a sympathetic ear, and she’d talk for hours with them — about family, memories and the things that mattered in their lives.
My grandmother was the “service provider,” but she received as much as she gave. She had no formal training or license, just the gift of connecting and the will to help.
I’ve been thinking about my grandmother lately because of our current crisis. Over the last month, I’ve heard more than once that the COVID-19 pandemic, as difficult as it is, will be followed by a second pandemic of anxiety, depression and post-traumatic stress, born of unprecedented economic dislocation and isolation. We are already seeing it.
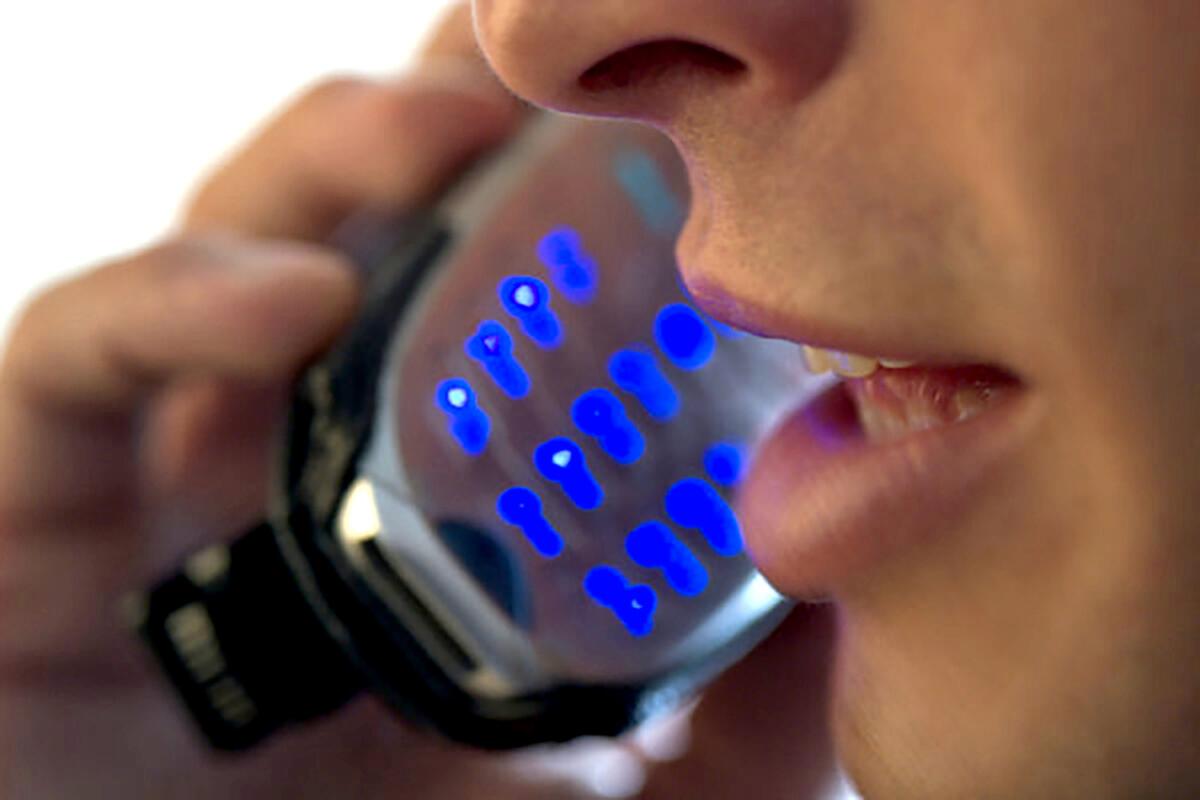
Calls to suicide hotlines have exploded. In Southern California, COVID-19-related calls to the Didi Hirsch Suicide Crisis Line went from a total of 21 in February to more than 1,800 in March. The Peer-Run Warm Line operated by the Mental Health Assn. of San Francisco has seen calls and chats surge and is logging as many as 274 calls a day, a 96% increase over its historic average and far exceeding its 160-call-a-day capacity.
And at a time when we desperately need our mental health professionals, surveys show that many of them face losing their jobs as clinics and practices are forced to close.
The mental health system has been broken for decades. Today, we can’t answer the most basic question asked by people in pain: “Where do I turn to get help for myself or my child, for my parent or partner?”
We desperately need to fix the fragmented system and ensure that support and care are there for those who need it. But my Grandma’s story reminds me of something that might help fill some gaps until then: mobilizing tens of thousands of people who want to help. Right now, in this time of need.
Some things are simple. We can all reach out to friends, neighbors and family who live alone or might be feeling lonely or vulnerable. But we also need a more organized response, one that involves training and deploying people, both volunteers and professionals, to reach out more broadly to those in need.
To get on track economically, we will need programs to help people who lost jobs during the crisis get back to work. Why not both train laypeople and enlist sidelined professionals to work supporting those in need? This kind of strategy helped us emerge from the Great Depression. We’ll need something similar today.
Gov. Newsom wisely created a California Health Corps to enable retired medical professionals to help address the physical healthcare needs of those hit by COVID-19. Why not the same for mental health? Here are four immediate steps California can take without any new state funding to boldly expand mental health services for our people.
First, expand the new California Health Corps to include a groundbreaking Mental Health Corps where mental health professionals working as volunteers or being paid by the state can be deployed to support those struggling with isolation and anxiety. Offer training to existing Health Corps members in a simple strategy called Mental Health First Aid to help them provide a full range of support and identify those in need of deeper assistance.
Second, increase state support for suicide, crisis and warm lines. For about $7 million, these services — currently swamped by a tsunami of need — could double their capacity to help people in crisis.
Third, contract with organizations such as the Trauma Resource Institute in Claremont to train laypeople in the community in techniques for coping with stress and trauma. The institute’s evidence-based methods, used across the U.S. and around the world to help people recover from disasters and traumatic experiences, help people cultivate their own resources and natural resiliency. For about $1 million, 1,000 people could be trained within a few weeks.
Fourth, highlight and promote the work of volunteer, mutual aid efforts such as USA COVID-19 Mutual Aid that facilitate people to help others in their community who need extra support to survive the crisis.
I was the Senate leader during the last budget crisis, so I know how tight money will be. But the investments I’m suggesting here are small and essential — and there are funding sources that could be tapped. The Mental Health Services Act fund has more than $700 million in reserve for a rainy day. The Federal Emergency Management Agency has been generous in reimbursing needed investments directly related to COVID-19. Let’s put some of this money to use.
The existing mental health system and its professional workforce cannot possibly meet the increased demand brought on by COVID-19. It is time to democratize the mental health provider movement in our country. We need an army of Henriettas to reach out to all those who are suffering. Those on both ends of the encounter will find it healing.
Darrell Steinberg is the mayor of Sacramento and founder of the Steinberg Institute, a statewide advocacy institute for mental health policy change.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.






