Op-Ed: Why politics may get in the way of the public accepting a COVID-19 vaccine

The key to defeating the COVID-19 pandemic may have less to do with vaccine science and logistics and more to do with public trust. Week after week, actions by Trump administration appointees have raised suspicions that political motives rather than science are driving decision-making in the development of the vaccine.
Events like these have shaken my faith — and the faith of many others — in two of the country’s most revered scientific institutions, the Centers for Disease Control and Prevention, which collects and analyzes healthcare data, and the Food and Drug Administration, which approves diagnostic tests and treatments.
As a longtime clinical scientist at the National Institutes of Health, I worked closely with many highly competent and hard-working CDC and FDA scientists. Until recently, both organizations enjoyed stellar international reputations for excellence, integrity and public health leadership. The coronavirus pandemic has thrown both agencies into disarray.
Recommendations by CDC scientists for reopening businesses and schools were withdrawn and weakened before being posted on the CDC website. Scientists fear that the revisions reflect the administration’s effort to spur the economy in an election year, even at the cost of spreading COVID. CDC guidance on aerosol transmission of the virus that would increase indoor distancing was also labeled a draft posted “in error” and removed from the website.
The CDC also revised guidelines — without public announcement and reportedly without the usual scientific review — to discourage testing of asymptomatic people despite unequivocal evidence that they readily spread the virus.
A long-established CDC surveillance system, the National Healthcare Safety Network had its COVID-19 module retired during the pandemic and replaced by a new data-collection process administered by a private contractor reporting directly to the CDC’s parent organization, the Department of Health and Human Services. Public health professionals have expressed concern about disruption of data collection as hospitals struggle with the new system and worry about possible manipulation and falsification of the collected information.
In addition, the HHS communications team has exerted unprecedented editorial control over the Morbidity and Mortality Weekly, the respected CDC publication. Political appointees with little scientific background have altered public health reports to align them with the administration’s coronavirus messaging. In one instance, HHS tried to suppress a report that questioned the effectiveness of the controversial malaria drug hydroxychloroquine, a treatment President Trump has promoted.
The CDC’s confused messaging has undermined its credibility. As a result, many of my colleagues who relied on CDC reports and recommendations have switched to other sources for unbiased COVID-19 information, such as the Johns Hopkins Coronavirus Resource Center.
The FDA’s loss of credibility has even more serious consequences for public health. At stake is the integrity of the FDA vaccine-appraisal process. The administration calls its effort to accelerate vaccine development Operation Warp Speed and has invested heavily in several vaccine candidates. Four have entered the final stages of clinical testing at an unprecedented pace. The FDA is responsible for approving these products.
The traditional FDA licensure procedure is lengthy and remains the gold standard for regulatory science. However, the FDA’s expedited process, known as “emergency use authorization,” requires much less evidence — but is generally reserved for extraordinary situations on a case-by-case basis.
Political pressures appear to have influenced repeated use of emergency authorization during the pandemic. The HHS secretary overrode objections from FDA scientists and revoked the agency’s authority to perform quality checks on SARS-CoV-2 laboratory tests. As a result, the FDA had to recall many inaccurate tests. The FDA has also issued emergency authorizations for two COVID-19 therapeutics that were promoted by the administration despite weak evidence. Now the FDA commissioner has announced that he would consider the emergency authorization for a vaccine before full evaluation of the clinical trials.
There is good reason to require full and transparent review of clinical trials data before approving a COVID-19 vaccine. Unlike therapeutics, which treat ill patients, millions of healthy subjects receive vaccines. They should be held to a higher standard of safety and efficacy. Several candidate vaccines rely upon new, clinically unproven technologies never tested in large-scale human trials. The FDA has already suspended one vaccine trial until severe adverse events can be fully evaluated.
Administration claims to the contrary, none of the trials has yet provided evidence of clinical benefit. There is no need to rush approvals as long as established preventive measures such as social distancing and masking can protect us until the trials can be properly completed and evaluated.
The FDA process includes a number of protections to prevent political interference with vaccine approval. Trial protocols do include an independent Data and Safety Monitoring Board that reviews and evaluates the study data during the trial. The FDA has also committed to discussing COVID-19 vaccine candidates with its externally constituted Vaccines and Related Biological Products Advisory Committee prior to issuing an emergency authorization. In an unprecedented move, nine chief executives of leading vaccine developers pledged “to uphold the integrity of the scientific process” as they proceed toward regulatory filings and approvals.
However, the president seems intent on announcing a vaccine before election day. The CDC has asked state governors to establish vaccine distribution facilities by Nov. 1, two days before the election. FDA leadership has promised that no vaccine would receive formal approval unless it met the agency’s published standards. The FDA commissioner has published more stringent emergency authorization standards, but the president has said the White House will not necessarily honor them. Besides, both the HHS secretary and the president can authorize a vaccine over the objections of experts, FDA officials — and even the pledge-signing vaccine manufacturers.
HHS has awarded $250 million to develop a public service campaign to “defeat despair and inspire hope” amid the pandemic. If the campaign educates the public about the need to accept a safe and effective vaccine, the money will be well spent. However, if it promotes a partially tested vaccine in the run-up to the election, it will further undermine public confidence.
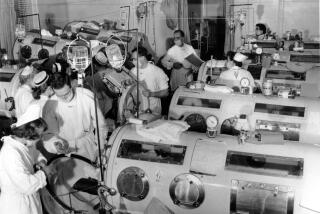
Vaccination has probably saved more lives and prevented more disease than any other public health measure. It works. I was vaccinated against smallpox in childhood and was an early recipient of the Salk polio vaccine. I get the flu vaccine each fall. Yet I would hesitate to be among the first to get a COVID- 19 vaccine if its availability is announced by emergency authorization shortly before the election.
We need to be confident that the vaccine has proved safe and effective after completion of rigorous clinical trials. A public relations campaign will not substitute for expert evaluation of data.
So much depends on public trust.
Dr. Harvey Klein is a scientist emeritus at the National Institutes of Health, where he was a senior investigator for 46 years. He co-chairs the World Health Organization Expert Committee on Biological Standardization.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.