Op-Ed: Telephone visits with doctors work. Don’t roll them back
At the beginning of the pandemic, a crucial change to Medi-Cal reimbursement policy made telehealth more accessible than ever for California’s most vulnerable populations. Visits conducted via telephone, online video or in person were to be covered equally.
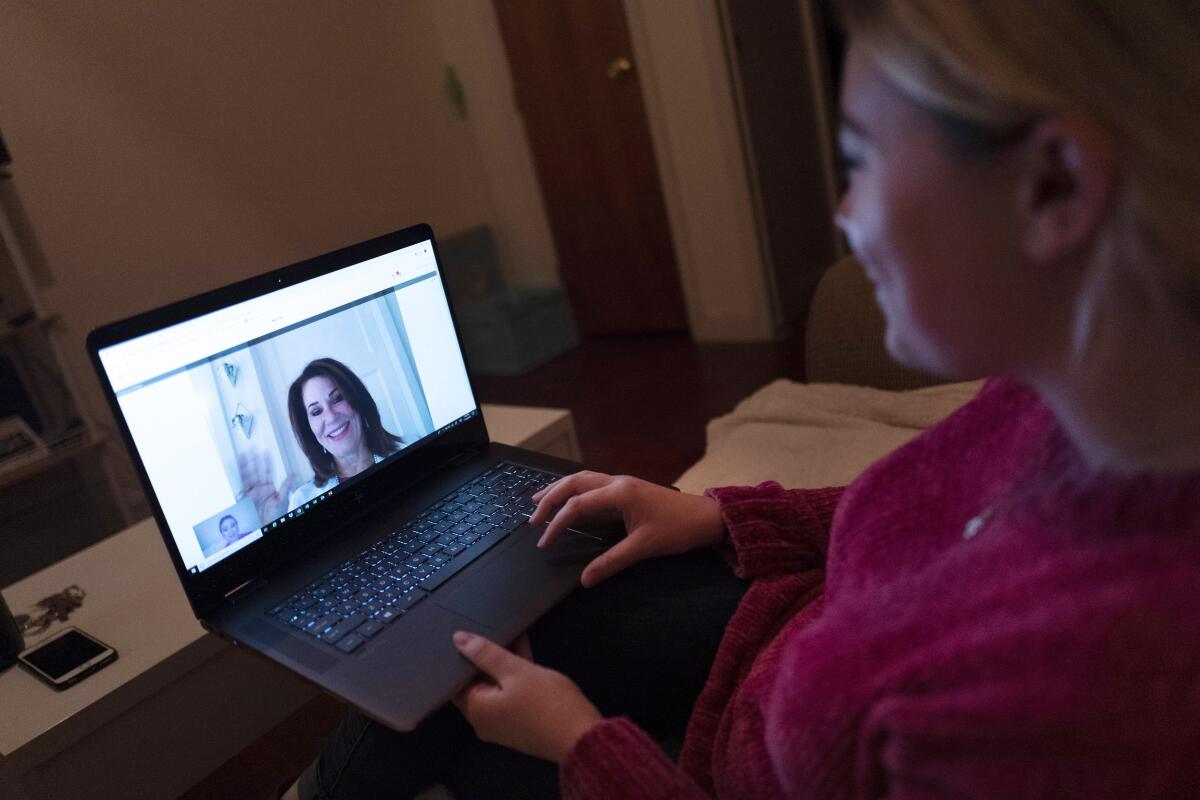
Our experience as clinicians during this time has shown us that putting telephone visits on equal benefit footing has dramatically expanded access to care without compromising quality. Yet the Centers for Medicare and Medicaid Services, along with California’s Department of Health Care Services, recently signaled they would reduce or eliminate reimbursement for audio-only visits.
The proposed change will unintentionally reinforce inequalities in the healthcare system. It will undo gains made in expanding access for the most vulnerable. To preserve these gains, equal payment for audio-only visits should be maintained.
Despite the major investments that have been made in video technology, most telehealth visits at safety-net healthcare providers — including the federally qualified health centers we work for — are conducted by telephone, without any video component. From March through August 2020, less than 4% of primary-care visits at similar health centers in California were conducted by video, compared with the nearly 50% that took place over the telephone.
In the communities we serve, we see that poor internet access accounts for much of the disparity. Just half of patients have access to Wi-Fi at home and nearly 60% use a cellphone, with limited data plans, as their main internet access point, according to a survey conducted by La Clinica de La Raza, a federally qualified health center with clinics in Alameda, Contra Costa and Solano counties. These findings mirror a similar study of patients served by the San Francisco safety net.
The move to telehealth has helped improve access for Californians with the most barriers to care. At West Oakland Health Council, another federally qualified health center, the expansion to telehealth is responsible for cutting the missed visit rate by half compared with before remote services were rolled out. Now only 15% of patients miss their appointments.
The survey of La Clinica de La Raza patients also found that more than half of them would prefer at least some of their visits to be remote. Evidence shows that telehealth use during the COVID-19 pandemic has reduced the barriers that families face in obtaining the care they need, including transportation, child care and work schedules. These barriers are not unique to care during the pandemic.
Despite findings that audio-only visits expand healthcare access, the Department of Health Care Services has indicated that audio-only visit payments will be eliminated or reduced compared with video or in-person visits, reasoning that telephone visits provide a lower quality of care. Not much data exist to show video provides higher quality of care, and little of it is conclusive.
Some studies have speculated that equal pay for all modes of telehealth will lead to overuse in an already strained state healthcare budget. The explanation given is that audio-only visits will be conducted in addition to in-person and video visits, making them superfluous. Yet, Medi-Cal patients are already chronically undertreated and deserve more care than they are currently receiving, regardless of how that care is given.
If DHCS officials truly believe that video provides higher-quality care than audio-only visits, a move to video should be accompanied by grants that support building technological infrastructure at safety-net clinics and digital literacy for their patients. The Federal Communications Commission has set up a similar program in the COVID-19 era that helps healthcare providers connect remote services to patients.
Rather than reducing care access options, DHCS should accelerate a planned transition to payment systems that reimburse for quality of care rather than quantity of care. The structures, called “alternative payment models,” will pay a set amount per patient per year for good health outcomes, rather than paying per visit. These models allow providers the flexibility to use whatever method of care — phone, digital outreach, community health workers, group visits or individual visits — that will result in the best outcomes for their patients.
The new DHCS policy may intend to improve quality of care. It does provide more options than were available pre-COVID, but it removes a crucial and much-used method for patients to connect with primary care that has proved extraordinarily useful. Safety-net clinics will have to fall back on approaches to care that don’t work as well for their patients.
Without strong data that support one approach to remote over another, the Department of Health Care Services should not move to change telehealth policy that is clearly working to expand access to care. Patients and their healthcare providers should get to choose what works best for them.
Sirina Keesara is an obstetrician-gynecologist at the West Oakland Health Council and an affiliate scholar at Stanford Medicine’s Clinical Excellence Research Center. Anastasia Coutinho is a family physician at La Clinica de la Raza in Contra Costa County.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.