Op-Ed: Too many of our pregnant patients refuse the COVID vaccine

In our high-risk pregnancy clinics there are three vaccine conversations that we have with patients regularly.
First, there are patients who are vaccinated for COVID-19 and counting down the days until they can schedule a booster shot. Then there are patients who will accept vaccines for influenza and Tdap (tetanus, diphtheria, pertussis), but not COVID-19.
The third conversation is with expectant mothers who not only decline a COVID-19 vaccination but also other vaccines recommended in pregnancy.
We have that third conversation at least once a day with patients, and we have run out of talking points. We tell these women that if they catch COVID-19, they will be 15 times more likely to die, 14 times more likely to be intubated, and many more times likely to have a preterm birth than those who are uninfected or who have been vaccinated.
A long-standing tradition of keeping pregnant women out of clinical trials is having serious consequences with regard to COVID-19.
No matter what we say, these patients fear that the COVID vaccine will harm them or their babies, despite the overwhelming evidence to the contrary. They repeatedly turn down the chance to protect themselves and their babies from the coronavirus.
Our patients are not alone in their hesitancy. According to the Centers for Disease Control and Prevention only 35.3% of pregnant women in the United States were vaccinated for COVID-19 as of Nov. 6. The numbers are even lower among pregnant Black women (20.6%) and Latina women (31.5%).
More than 24,700 pregnant women in the United States have been hospitalized with COVID-19. As of Nov. 8, 227 have died from COVID nationwide. The deadliest month for pregnant women during the pandemic was not in 2020, before vaccines were available, but this past August, during the Delta variant surge.
These numbers do not sway our pregnant patients to comply with our recommendation for vaccination.
When vaccines first were approved our patients’ fears were understandable. Because pregnant women were excluded from early COVID-19 vaccine trials, we OB-GYNs had little data to reassure them that they and their babies would be safe when vaccines first became available.
Once compelling data arrived showing that COVID-19 vaccines are safe for pregnant individuals and confer protection to newborns, many expectant mothers and women planning to get pregnant had already made up their minds that the vaccines were dangerous, and it was too late to convince them otherwise.
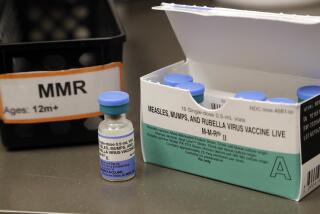
The Centers for Disease Control and Prevention is urging all pregnant women to get vaccinated against COVID-19.
We cannot take our vaccine-hesitant patients on a tour of the ICU, giving them a chance to experience the trepidation we feel every time we put on specialized protective equipment just to enter the room of a pregnant patient sick with COVID.
There is no way to express to them the exhaustion and the anguish of trying to find COVID-positive pregnant patients a hospital bed and a nurse to provide care when calls from community hospitals come in with a patient they need to transfer.
There is no way to convey the sense of relief our entire team feels when we successfully discharge a mother who has survived COVID and myriad other complications — though that feeling is inexorably bound to the frustration of knowing that a vaccination could’ve prevented her admission altogether.
Hospital providers and staff are traumatized, overtaxed and in short supply. We know that when a pregnant mother arrives in the hospital with COVID, it may be only a matter of hours before she deteriorates and needs an emergency caesarean section.
During this surgery, at least a dozen people — including the surgical team, neonatal-care specialists and anesthesiologists — arrive in an operating room empty of the typical equipment to avoid contaminating surgical supplies beyond the ones needed for this procedure with the virus. We leave our ID badges and pagers outside. We put on N-95 masks and positive air-purifying respirators hoods.
It is difficult to talk, breathe or hear each other. A team clears the elevators and hallways to transfer the patient to the operating room, where we wait. When the transfer team leaves, they literally seal the doors shut, with us inside.
For more than 18 months we’ve done this again and again.
One additional challenge for our fragile healthcare system is that we are also in a baby boom: Our hospital in Seattle had record child deliveries this summer. The contrast between our healthy, normal deliveries and our dire COVID deliveries, happening simultaneously, is almost too much to reconcile.
But until pregnant women are vaccinated against COVID, we will need to do it all over again tomorrow.
Alyssa Stephenson-Famy is an associate professor of obstetrics and gynecology, specializing in high-risk pregnancies, at the University of Washington School of Medicine. Linda Eckert is a professor of obstetrics and gynecology, specializing in infectious diseases and immunization, also at the University of Washington School of Medicine.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.