Coronavirus Today: The sacrifices of nurses
Good evening. I’m Amina Khan, and it’s Tuesday, Oct. 27. Here’s what’s happening with the coronavirus in California and beyond.
The healthcare workers on the front lines of the COVID-19 pandemic all face risks to some extent, but a new study shows that they don’t bear the risks equally. In the early months of the outbreak in the U.S., nurses were far more likely than doctors to be hospitalized with COVID-19 and to die of the disease, according to a new study prepared for the Centers for Disease Control and Prevention.
In part, that disparity reflects differences in the nature of the work done by nurses and doctors. The findings also highlight some of the larger health disparities faced by people of color across the United States, my colleague Melissa Healy reports.
Researchers scoured a sample of 6,760 adults hospitalized for COVID-19 between March 1 and May 31 and found that nearly 6% of those patients were healthcare workers. Just over two-thirds of them were in jobs where they would probably have direct contact with patients — especially nursing.
That may seem to make sense on an intuitive level: Nurses spend more time in close contact with sick patients compared with the relatively brief visits of doctors. In addition to tasks like taking vital signs and changing IVs, they are the ones who sit by patients’ bedsides in lieu of families, or who held phones so that a patient could connect with loved ones barred from visiting in person.
“This is not rocket science,” said healthcare expert Barbara Resnick of the University of Maryland’s School of Nursing, who was not involved in the new study. “Nurses are providing direct care to patients, and you have to be up close and personal for a lot of what they do. They spend the most time with patients, especially the nursing assistants. Bathing, dressing and giving medications — you can’t do that from six feet away.”
Those longer periods of contact potentially expose nurses to higher doses of virus, which is a factor in causing more severe illness, experts say.
These healthcare workers were mostly female and generally younger than the larger pool of hospitalized COVID-19 patients. And yet they became seriously ill and died at rates that were similar to those in older patients. The median age of the hospitalized healthcare workers was 49, 13 years younger than the median age for the entire group of 6,760 COVID-19 patients. And although men who develop severe cases of COVID-19 generally outnumber women, 72% of the healthcare workers hospitalized for COVID-19 were female, reflecting women’s larger numbers in nursing and related healthcare fields.
But the workers did fit into other circles on the Venn diagram of COVID-19 risk factors. Nine out of 10 had an underlying health condition that increased their vulnerability, such as hypertension, asthma, heart disease or diabetes. Almost three-quarters were identified as obese, a powerful risk factor for a serious case of COVID-19. And more than half — 52% — were Black Americans.
In part because Black people are heavily represented among essential workers, coronavirus infection rates have run three times higher in counties with predominantly Black populations than in counties that are predominantly white, and COVID-19 death rates are six times higher. In addition, Black Americans are subject to health disparities that lead to higher rates of diabetes, asthma, hypertension and obesity. These inequities helped drive the disproportionate death rates.
By the numbers
California cases and deaths as of 6:34 p.m. PDT Tuesday:
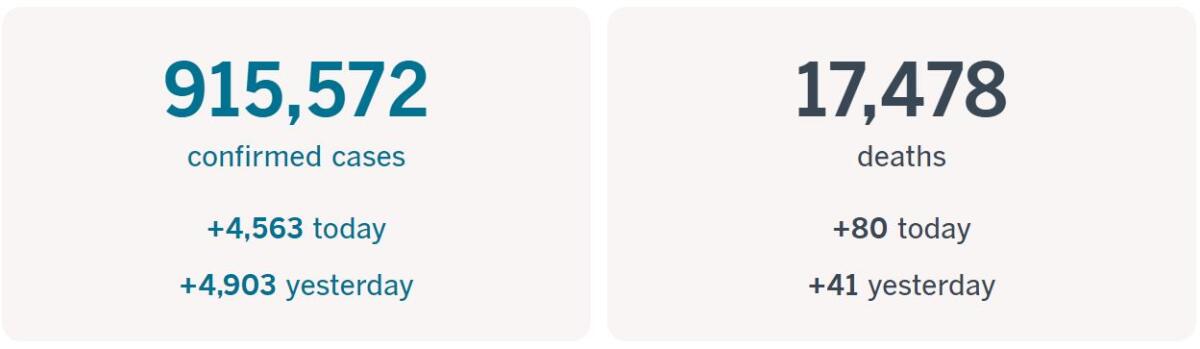
Track the latest numbers and how they break down in California with our graphics.
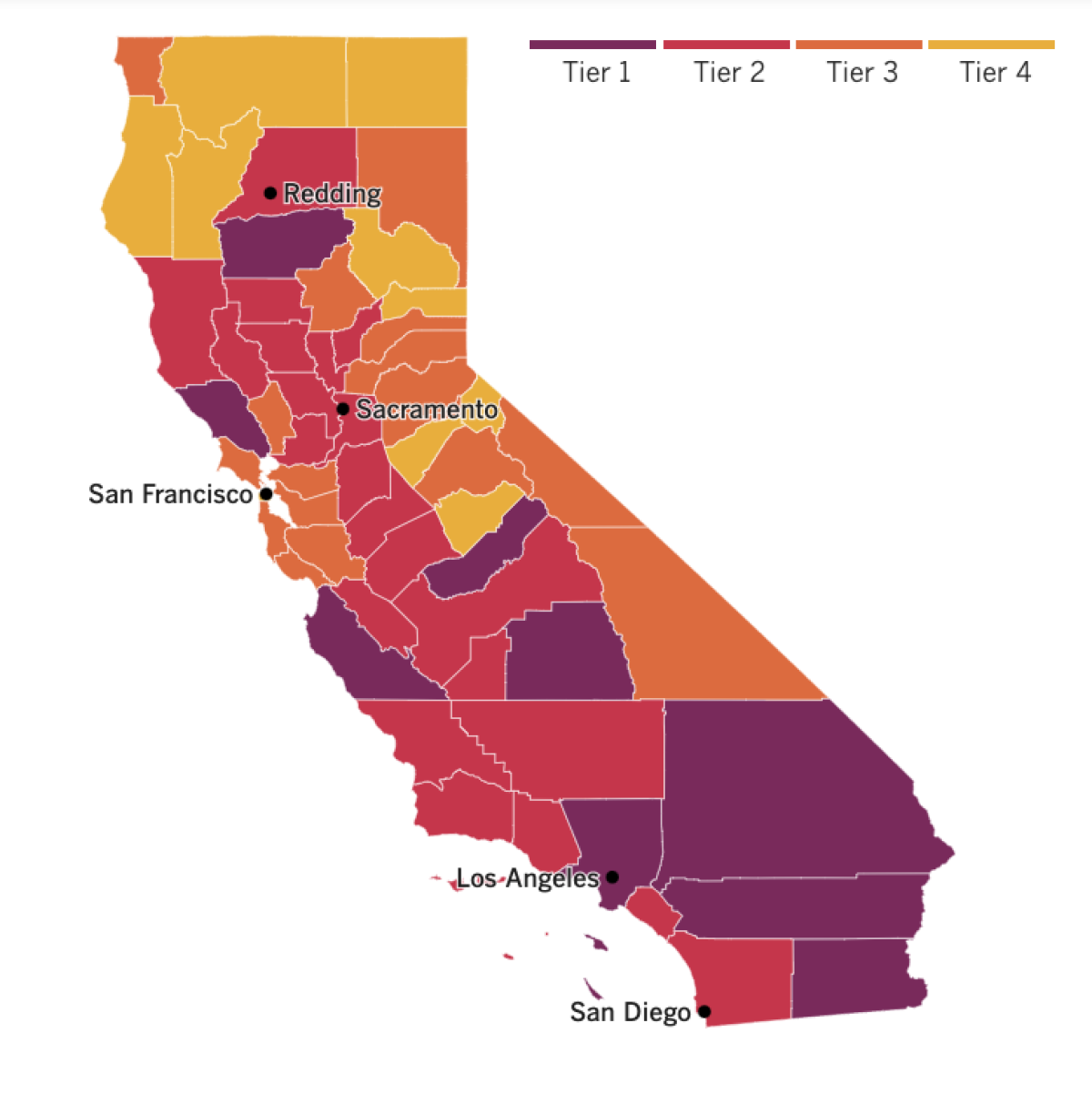
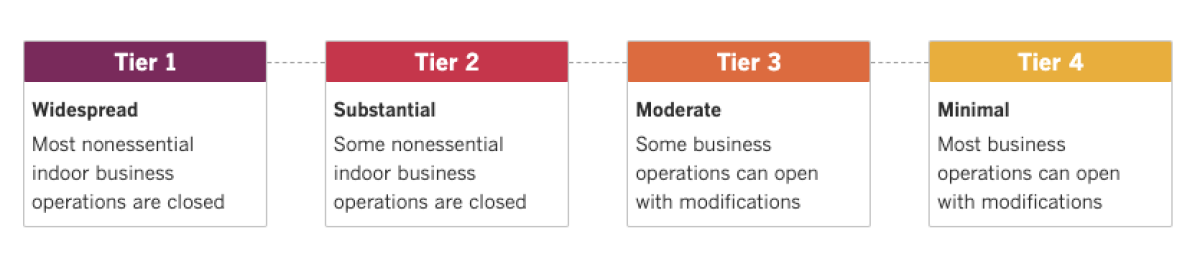
See the current status of California’s reopening, county by county, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Across California
Tuesday is moving day for counties hoping to progress up the state’s color-coded, four-tier reopening road map. Two counties graduated from the most restrictive purple Tier 1 into the red Tier 2 — but Los Angeles County wasn’t one of them.
Indeed, four Southern California counties — Los Angeles, San Bernardino, Riverside and Imperial — ranked among the state’s top five for the average number of new daily infections per 100,000 residents over the last week, according to The Times’ coronavirus tracker.
New cases in Los Angeles County jumped to an average of 111.3 per 100,000 residents last week, up from 63.4 per 100,000 residents the week before. The average case rate climbed from 77.5 to 140.3 in San Bernardino and from 94.4 to 111.5 in Riverside, while in Imperial new cases soared from an average of 141.5 per 100,000 residents to 225.8.
The increases in Southern California were contributing to an overall rise statewide. According to the most recent available state data, the latest seven-day average of new cases throughout the state is 4,303 — notably higher than the 14-day average of 3,699.
The rise is “a cause for concern,” L.A. County Public Health Director Barbara Ferrer said Monday, and came about because “of decisions we collectively made two to three weeks ago, and the action we’re taking today will influence whether we continue our recovery journey, we stall, or we step backward.”
UCLA announced that remote learning will continue in the winter quarter even as other UC campuses continue to assess plans for the new year. While there will be some exceptions for students who attend hybrid courses, such as labs and studio art classes, instruction will largely remain online through March 19, when the winter quarter ends.
“We were hopeful that we could expand instruction to include more in-person classes next quarter, but given the continued spread of COVID-19, and in line with strict county public health mandates, we must maintain a reduced population and limit person-to-person contact on campus,” Executive Vice Chancellor and Provost Emily Carter said in a statement.
COVID-19 has forced employers to cut hundreds of thousands of jobs in Hollywood, but there’s at least one show business position that the pandemic has actually created: the COVID-19 compliance supervisor. This supervisor is responsible for making sure TV and film productions are following the protocols put in place to keep workers safe despite the outbreak.
The newly created role is the result of an agreement last month by entertainment unions and an association of film and television producers that allowed Hollywood to get back to business. The film and TV industry has been slowly gearing up since June after a near-total shutdown in March.
The job of COVID-19 compliance supervisor comes with a significant set of responsibilities: sanitation, testing and enforcing rules on distancing. Supervisors have to make sure cast and crew are split into different zones based on the frequency of testing and their ability to wear masks. The supervisor is also responsible for training other crew members so they can pass on safety instructions to their sections, and they must be available during all working hours.
With great responsibility comes great power — the power to stop a production if there are safety concerns, and the power to potentially fire people who violate safety protocols.
Because there aren’t well-defined qualifications or required training, compliance supervisors have so far come from different backgrounds, such as medicine, film production or set safety. Many of them once worked as set medics. And they’re in high demand. Jessica Lesley started a company that provides COVID-19 safety services to the industry. “I’ve been going since June, and I’ve been extremely busy,” she said.
Resources
— For general safety, wash your hands for at least 20 seconds (here’s a super-fun how-to video). Stop touching your face, and keep your phone clean. Practice social distancing, maintaining a six-foot radius of personal space in public. And wear a mask if you leave home. Here’s how to do it right.
— Watch for symptoms including fever, cough, shortness of breath, chills, repeated shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. If you’re worried you might be infected, call your doctor or urgent care clinic before going there.
— Need a COVID-19 test? Here’s how to receive a free test if you’re in L.A. County. And here’s a map of testing sites across California.
— Here’s how to care for someone with COVID-19, from monitoring their symptoms to preventing the virus’ spread.
— If your job has been affected by the pandemic, here’s how to file for unemployment.
— Here are some free resources for restaurant workers and entertainment industry professionals having trouble making ends meet.
— Advice for helping kids navigate pandemic life includes being honest about uncertainties, acknowledging their feelings and sticking to a routine. Here’s guidance from the CDC.
— In need of mental health services? Here are resources for coping during the crisis from the CDC and the L.A. County Department of Mental Health. L.A. County residents can also call (800) 854-7771 or text “LA” to 741741.
— For domestic violence victims, the pandemic can pose a “worst-case scenario,” advocates say. If you or someone you know is experiencing such abuse, call the National Domestic Violence Hotline at 1-800-799-SAFE (7233) or L.A. County’s hotline at 1-800-978-3600. Here are more ways to get help.
Around the nation and the world
Here’s another way the pandemic may change the outcome of the presidential election: by sending college students attending swing-state universities back to their own home states.
Campuses have often served as centers of liberal political activism and get-out-the-vote efforts, my colleague Kurtis Lee writes. Together, those tendencies have allowed Democrats to win elections in swing states.
But that was before the coronavirus hit. This fall, colleges and universities reportedly saw a 4% drop in enrollment — and in the Midwest, where several swing states lie, the drop was 6%.
“In a tight race, the absence of college students could easily tilt a state,” said Nathan L. Gonzales, editor of Inside Elections, a nonpartisan group that analyzes federal and state contests. “Just like suburban women, or rural voters, every vote matters.”
Bryce Neels of San Diego is one of those would-be swing state voters. The 21-year-old University of Wisconsin junior said he chose that school in part because the campus lies in a swing state. Now that he’s back in San Diego and taking classes on Zoom, he had no choice but to cast his vote in California, which his favored candidate, Joe Biden, is expected to take in a landslide vote.
“Any other election year, I would have been there,” he said. “But 2020 is clearly different.”
Speaking of Wisconsin, the U.S. Supreme Court on Monday refused to extend an election-day deadline for mail-in ballots in the Badger State. That means that mail ballots will have to be received by election day in order to count.
Democrats and voting rights advocates unsuccessfully argued that ballots postmarked by election day should be counted if they were received in the next six days. Justice Elena Kagan cited the coronavirus in her dissent: “As the COVID pandemic rages, the court has failed to adequately protect the nation’s voters. Tens of thousands of Wisconsinites, through no fault of their own, may receive their mail ballots too late to return them by election day.”
In Rome, Pope Francis has been inconsistent about wearing a mask, donning it occasionally but often forgoing it, even indoors. Those practices have raised eyebrows among members of the Vatican coronavirus commission that he appointed to deal with the pandemic and its fallout.
Because the pope is 83 and is missing a part of his lung — it was removed after an illness in his youth — he would be at high risk for complications if he were to become infected, the Rev. Augusto Zampini, one of the commission’s key members, acknowledged Tuesday.
“He has started to use the mask now,” Zampini said in response to reporters’ questions. “And I hope he will use it in the general audiences, when he is close to the people. If you’re in an open space, we know that it’s different. But, well, we are working on that.”
The comments came after a recent rise in infections in the Vatican: Thirteen Swiss Guards and a resident of the quarters where Francis lives have tested positive. Zampini said that while they’re worried, the infections have helped the Vatican better understand the dangers posed by the coronavirus to the world at large.
Your questions answered
Today’s question comes from readers who want to know: How does train travel compare with air and car travel in terms of coronavirus risk?
At this point, given how little we really know about transmission rates in these different travel contexts, it’s impossible to give a definitive answer on whether cars, trains or planes are your most palatable option in terms of COVID-19 risk, says Tanjala Purnell, an epidemiologist at Johns Hopkins Bloomberg School of Public Health.
Even if we had better data, there are just too many variables to give a one-size-fits all answer. For example, a car ride might seem safer than air travel, since you’re not sharing public spaces — but what if that trip takes 16 hours, involving multiple stops for gas and food and perhaps an overnight hotel stay?
“The short and long answer is we don’t know enough — and if anyone says that we do, then that’s probably someone that’s not thinking about all the different scenarios,” Purnell said.
That said, she added, it’s definitely worth thinking about the risks associated with each form of travel in the context of your personal travel plans. The Centers for Disease Control and Prevention breaks them down here.
Air travel puts passengers in contact with other people and shared surfaces at the airport and in the airplane cabin. (That’s not to mention the exposure you might get from a ride share on your way to and from the airport.) The CDC says most viruses and other germs don’t spread easily on flights because of how air circulates and is filtered.
Car travel doesn’t involve that set of risks. But there are others involved with stops along the way.
My colleague Mary Forgione recently wrote about the steps Amtrak says it’s taking to reduce COVID-19 exposure risk on its train lines. Thanksgiving riders will need to reserve a seat, including for the Pacific Surfliner in Southern California. The rail company is selling a limited number of tickets to allow for social distancing in its cars, and it won’t charge change fees on reservations made by Dec. 31.
Amtrak also offers roomettes that can accommodate two passengers and larger bedrooms that can fit full families. The bedrooms also have a private toilet, which theoretically allow you to sequester yourself fairly well. As always, mask-wearing and maintaining at least a six-foot distance from other passengers is key.
Still, the CDC recommends avoiding travel during these pandemic times, as it raises your risk of exposure relative to staying home. Any form of travel comes with some risk.
Our reporters covering the coronavirus outbreak want to hear from you. Email us your questions, and we’ll do our best to answer them. You can find more answers in our Frequently Asked Questions roundup and in our reopening tracker.
For the most up-to-date coronavirus coverage from The Times over the weekend, visit our homepage and our Health section, sign up for our breaking news alerts, and follow us on Twitter and on Instagram.




