Coronavirus Today: ‘Normality’ in 2022?
Good evening. I’m Amina Khan, and it’s Thursday, Oct. 29. Here’s what’s happening with the coronavirus in California and beyond.
If you’re like me, you’re looking forward to a moment in the hopefully not-too-distant future when a vaccine becomes available to the general public. Everything will change, I dare to think, as soon as the vaccine becomes available.
Well, Dr. Anthony Fauci, our nation’s top infectious-disease expert, is here to splash a little cold wet reality all over my fantasy. Getting a vaccine is not automatically and immediately going to fix all of our problems. We may not start to feel anything like “normal” until 2022, he said. And that’s only if the U.S. gets a significant share of its residents vaccinated around mid-2021.
“I think it will be easily by the end of 2021 — and perhaps even into the next year — before we start having some semblance of normality,” Fauci said during an online discussion hosted by an Australian university.
Some of the hallmarks of the Before Times that we yearn for — bustling restaurants, packed movie theaters, candle-blowing at a birthday party — may not be possible without risking a super-spreading event (one in which a large number of people are infected). Recent research has found that a few super-spreading individuals are responsible for a disproportionate share of new coronavirus infections.
Of course, normality itself may have shifted away from what you may remember of the Before Times. Fauci said he believed that wearing masks would continue to be commonplace in the U.S. (as it has been in many parts of Asia for decades).
Fauci warned that the U.S. was heading down a dangerous path, what with more than 228,000 deaths from COVID-19 and, recently, 83,000 new infections in a single day. That’s more than eight times as high as it should be: Fauci previously said that the U.S. should aim for fewer than 10,000 new cases a day as we head into winter.
“That is very troubling,” Fauci said. “We’ve got to do better than that.”
If the U.S. is going in the wrong direction, it has much to do with the country’s fragmented response to the pandemic. Different states implemented differing control strategies, which made management far more difficult. This problem became exceedingly clear when Fauci and Dr. Deborah Birx, the White House coronavirus response coordinator, developed guidelines to try to reopen the economy.
“It was like a free-for-all,” Fauci said. “Some states jumped over one benchmark to the other. And some states tried to do it well, but yet when you looked at the TV screen, you’d see people crowded at bars, with no masks, just essentially causing super-spreading” despite federal guidelines for wearing masks, keeping physically distant and avoiding crowded settings. “If everybody had done that uniformly,” he added, “I don’t think we would be in the position we’re in right now.”
A uniform policy is key to managing these border-crossing outbreaks, officials said. For example, in Melbourne, Australia, residents almost universally wear masks, because people who don’t wear them outside are fined $1,000, another panelist in the discussion said.
Fauci said he wished that mentality could be transplanted to the U.S. He and many other health experts are increasingly discussing the need for some type of nationwide mask mandate.
By the numbers
California cases and deaths as of 4:46 p.m. PDT Thursday:
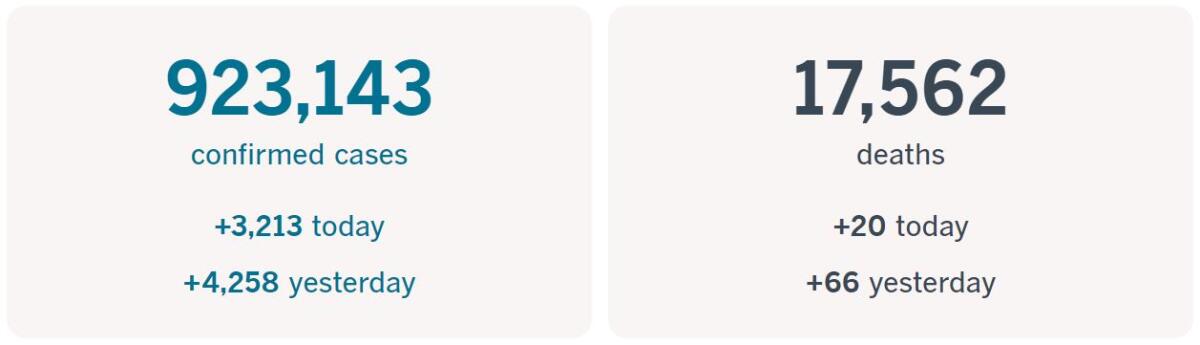
Track the latest numbers and how they break down in California with our graphics.
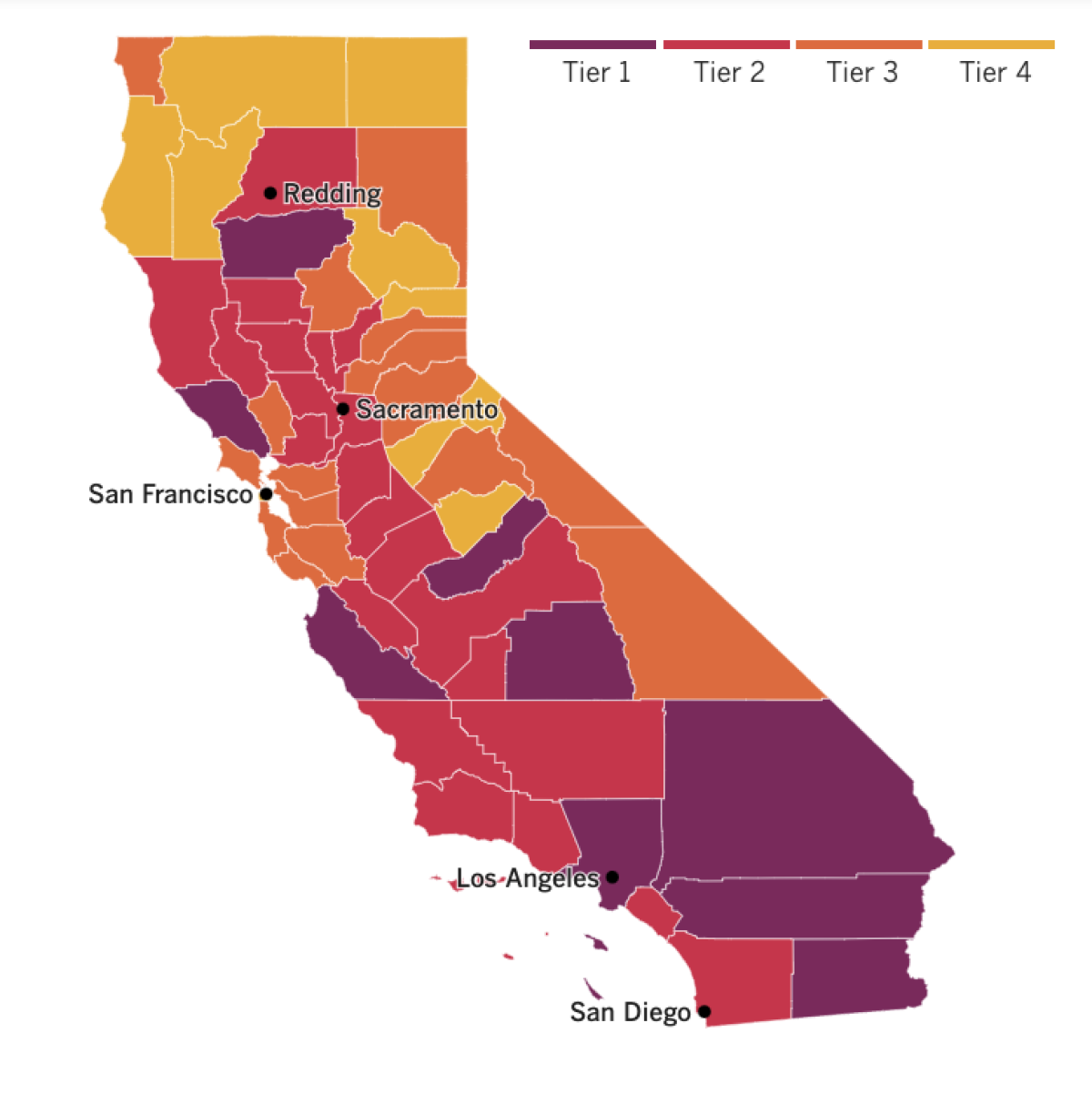
See the current status of California’s reopening, county by county, with our tracker.

Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Across California
The spread of the coronavirus appears to be picking up again in Los Angeles. The county reported 1,745 new cases Thursday and 19 new deaths — the highest one-day increase in cases since August (not including increases that were due to a reporting backlog). If the area does see another spike like the one experienced this summer, it could endanger nascent efforts to reopen schools and businesses.
The new numbers come on the heels of the Dodgers’ World Series win and the Lakers’ NBA Finals win this month. Officials have worried that the coronavirus is spreading from social gatherings of celebrating fans.
In fact, if you were out celebrating the Lakers’ or Dodgers’ championship wins, do yourself and your fellow Angelenos a solid and get tested for the coronavirus, officials say. “For those who went to the streets to celebrate … and were around strangers in an unsafe environment, please get tested and stay isolated for 14 days per the county’s Department of Public Health advice,” Los Angeles Mayor Eric Garcetti said Wednesday.
Garcetti and county health officials have reasons to worry. Thousands flocked to the streets Tuesday after the Boys in Blue took home the World Series championship, even though health officials urged euphoric fans to stay home.
Sports columnist Bill Plaschke has some strong words for Dodgers third baseman Justin Turner and his decision to run onto the field, hug his teammates and remove his mask for group photos after testing positive for the coronavirus. “In the interest of common sense, millions of other Americans have been purposely absent for many deeply personal events, canceling weddings, postponing funerals, missing births,” Plaschke wrote. “Justin Turner wouldn’t skip a trophy celebration.”
Doing so endangered other players, other colleagues and their wives and children, including at least one pregnant woman. Because of this, an otherwise triumphant moment for Los Angeles “has been shaded in shame,” he wrote.
In this moment of victory, Turner could have set an example for those watching by remaining in isolation (as required by Major League Baseball), modeling responsibility and teaching a hard lesson. “Instead, he put a lot of people around him at risk,” said Anne Rimoin, a lifelong Dodgers fan and UCLA epidemiology professor. “And now he’s an example to a lot of people: ‘If Justin Turner can do it, why can’t I?’ And that’s a real problem.”
Plaschke himself battled COVID-19, so he knows what the consequences of infection can be.
While COVID-19 has become an unavoidable talking point in the presidential race, it has left its mark on some of California’s most contentious local elections too. Pundits were shocked two years ago when Democrat Harley Rouda defeated longtime Republican congressman Dana Rohrabacher in the 48th Congressional District. Now, there’s a chance the seat could flip back to red as Republican Orange County Supervisor Michelle Steel challenges Rouda.
A complicated mix of political ingredients plays into this race, and the pandemic has turned out to be a defining one. Steel has cultivated ties to President Trump and won praise from other Republicans for pushing to reopen local businesses in the midst of the pandemic. Rouda, meanwhile, argued that Steel has not been taking the pandemic seriously in her role as a supervisor, pointing to a recent fundraiser where she and others gathered indoors without masks.
The pandemic has had earth-shaking consequences for small businesses in Southern California. Some have been able to adapt and survive, often going through transformative changes; others have died as their clients have dried up. The Times’ Business team brings you stories of four small businesses that have so far made it, and three that haven’t. Among them: an event planner who turned to yoga retreats, a financial adviser who now holds her client meetings in her driveway, an LGBTQ-owned and operated coffee shop and a well-loved Middle Eastern restaurant.
Here’s a handy public service announcement as our pandemic-tinted election draws closer by the day: If you are in the hospital, you can still vote. California law protects the rights of voters who are in the hospital or other care facilities, and you are probably eligible to cast an emergency ballot. Read more here.
Resources
— For general safety, wash your hands for at least 20 seconds (here’s a super-fun how-to video). Stop touching your face, and keep your phone clean. Practice social distancing, maintaining a six-foot radius of personal space in public. And wear a mask if you leave home. Here’s how to do it right.
— Watch for symptoms including fever, cough, shortness of breath, chills, repeated shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. If you’re worried you might be infected, call your doctor or urgent care clinic before going there.
— Need a COVID-19 test? Here’s how to receive a free test if you’re in L.A. County. And here’s a map of testing sites across California.
— Here’s how to care for someone with COVID-19, from monitoring their symptoms to preventing the virus’ spread.
— If your job has been affected by the pandemic, here’s how to file for unemployment.
— Here are some free resources for restaurant workers and entertainment industry professionals having trouble making ends meet.
— Advice for helping kids navigate pandemic life includes being honest about uncertainties, acknowledging their feelings and sticking to a routine. Here’s guidance from the CDC.
— In need of mental health services? Here are resources for coping during the crisis from the CDC and the L.A. County Department of Mental Health. L.A. County residents can also call (800) 854-7771 or text “LA” to 741741.
— For domestic violence victims, the pandemic can pose a “worst-case scenario,” advocates say. If you or someone you know is experiencing such abuse, call the National Domestic Violence Hotline at 1-800-799-SAFE (7233) or L.A. County’s hotline at 1-800-978-3600. Here are more ways to get help.
Around the nation and the world
If you want to know how COVID-19 came to cause more than 227,000 deaths in the U.S., you could seek answers from infectious-disease experts, epidemiologists or front-line medical workers. Or you could turn to social scientists.
In a new report, political scientists, social psychologists, sociologists and others explain how America’s toxic degree of partisanship has hindered efforts to confront the pandemic. That’s how the decision about whether to wear a mask to prevent the coronavirus’ spread morphed from a question of public health into a political statement. COVID-19 isn’t the only inherently apolitical threat to tie the country up in partisan knots; the report also cites climate change and the federal debt. The key to all this dysfunction is the tendency to view one’s political rivals as not merely misguided but downright evil.
The authors of the report call this woeful state of affairs “political sectarianism,” and the pandemic has made its effects crystal clear. Now that masks have come to be associated with Democrats, Republicans are less inclined to wear them. “The result has been lethal and expensive for Americans across the political spectrum,” the experts write.
Business columnist David Lazarus has a bone to pick with Trump over the president’s accusations that Democratic challenger Joe Biden would allow for “socialized medicine.” But Trump has already made major socialized-medicine moves of his own, announcing his administration will pay $375 million for 300,000 doses of an experimental COVID-19 drug from Eli Lilly & Co. — “spending a ton of your money” to buy a treatment whose true efficacy isn’t yet clear, Lazarus writes.
That’s how it should be, Lazarus argues; vaccines are not profitable for companies, which is why the government must step in. “The role of the government here is to fix a market failure,” said Scott Barkowski, a healthcare economist at Clemson University. And of course, we’re already benefiting from socialized medicine, Lazarus writes. “Medicare, Medicaid, veterans’ assistance, programs for healthy kids — these are all examples of socialized medicine, and somehow we’ve avoided turning into the Soviet Union.”
In Europe, the Vatican has ended Pope Francis’ general audiences with the public after a confirmed infection at last week’s audience. Instead, he’ll be returning to livestreaming his weekly catechism lessons from his library in the Apostolic Palace, just as he did during the Vatican’s earlier coronavirus lockdown this spring and summer.
Francis had resumed the sessions Sept. 2 in a Vatican courtyard with limited numbers of attendees. But the pope had been criticized for not wearing a mask, particularly when greeting prelates at the end of his audiences. Several Swiss Guards at the Vatican have also tested positive for the virus. The decision comes amid a serious resurgence of infections in Italy, which was the first country in Europe to be hit hard by COVID-19.
And France announced a full lockdown for the second time this year while German officials imposed a partial four-week lockdown Wednesday, all in an effort to stop a fresh flood of coronavirus cases. “We are deep in the second wave,” European Commission President Ursula von der Leyen told reporters in Brussels. “I think that this year’s Christmas will be a different Christmas.”
Your questions answered
Today’s question comes from a reader who wants to know: What is the purpose of face shields? Do they replace masks?
The short answer to that second question is no, they do not replace your mask, says Neysa P. Ernst, nurse manager for the Biocontainment Unit at Johns Hopkins Hospital, who fields this question from patients every day.
“Face shields alone do not protect a person from COVID-19 transmission,” Ernst said. “COVID-19 is transmitted when an infected person sends droplets into the air by coughing, sneezing, singing or shouting. A face shield will protect your eyes but not provide complete coverage for your nose or mouth. Infected droplets can then be inhaled via the exposed nose or mouth.”
Jade Flinn, a nurse educator for the biocontainment unit, agreed.
“Face shields should not be used in lieu of face masks,” she said. “Face shields should be viewed as a protective addition to face masks to protect mucous membranes and protect the face mask from direct contamination.”
The federal Centers for Disease Control and Prevention does not recommend the use of face shields in place of masks. But it does recognize that a mask may not be feasible in every situation — for example, for some people who are deaf or hard of hearing or who care for or interact with someone who is. Evidence regarding face shields is limited, but the data that do exist indicate that in these instances, hooded face shields or face shields that wrap around the sides of the wearer’s face and extend below the chin may provide “better source control” than others.
Our reporters covering the coronavirus outbreak want to hear from you. Email us your questions, and we’ll do our best to answer them. You can find more answers in our Frequently Asked Questions roundup and in our reopening tracker.
For the most up-to-date coronavirus coverage from The Times over the weekend, visit our homepage and our Health section, sign up for our breaking news alerts, and follow us on Twitter and on Instagram.