Coronavirus Today: Vaccines, trust and Latinos
- Share via
Good evening. I’m Amina Khan, and it’s Wednesday, Dec. 9. Here’s what’s happening with the coronavirus in California and beyond.
With the first COVID-19 vaccine on the horizon, some of us may be allowing ourselves to fantasize about a future lived free of pandemic restrictions. But about 70% of the population will need to get vaccinated in order to attain herd immunity and stop the coronavirus from spreading out of control. Public health officials are increasingly concerned that vaccine hesitancy will keep that from happening — particularly among people of color, who have expressed higher levels of reluctance to get vaccinated than their white peers.
That’s certainly the case among California’s Latino community. In an October survey, only about half the state’s Latino population said they would probably take a COVID-19 vaccine, far fewer than public health officials would like. And while it isn’t the lowest level — fewer than 30% of Black Californians said they would take it — it’s a big deal, because Latinos make up 40% of the state’s population, represent 58% of its coronavirus cases and account for 48% of its COVID-19 deaths.
“California’s fate, to no small degree, rests on how Latino residents fare during and after this pandemic,” my colleague Brittny Mejia writes.
In Los Angeles County, Latinos are now becoming infected at more than twice the rate of white residents, data show. That disproportionate toll is partly due to the fact that Latinos are overly represented among “essential workers,” who are more likely to be exposed to the virus.
Mejia spoke to Latinos up and down Pacific Boulevard in Huntington Park to see how they were feeling about taking the vaccine. Silvia Orellana, a perfume shop owner, told Mejia she sees the destructive forces of the virus in the anemic foot traffic outside her store. Orellana even had a recent scare where she thought she’d been infected. (It turned out to be the flu.)
Still, the 45-year-old said she wouldn’t take the COVID-19 vaccine. Three years ago, she suffered a fever, chills and pain in her bones after a flu shot, and she doesn’t want to take a chance on another vaccine.
The Latinx experience chronicled
Get the Latinx Files newsletter for stories that capture the multitudes within our communities.
You may occasionally receive promotional content from the Los Angeles Times.
That sentiment was echoed by many Latinos, Mejia writes, though it angers others, like Berta Calderon, who works across the street from Orellana. A longtime friend of hers died of COVID-19 in June, and children in her catechism class have lost parents. “It’s necessary that we get vaccinated,” Calderon said. “I’m going to get it as soon as I can.”
Overall, experts say it’s going to take time to build the trust needed to get enough people to sign up for the vaccine. And doing so will require enlisting trusted community messengers.
Building that trust is what compelled Alejandra Sotelo-Solis, the mayor of National City, to enter the UC San Diego Health COVID-19 vaccine trial last month.
“I think that I’m in this unique position to where I can say, ‘Look, I went through the process, and this is what you can expect,’” said Sotelo-Solis. Her decision to join the trial was met with skepticism by some relatives who asked: Why did it have to be her?
She had a simple answer: “Why not me?”
By the numbers
California cases and deaths as of 5:30 p.m. PST Wednesday:
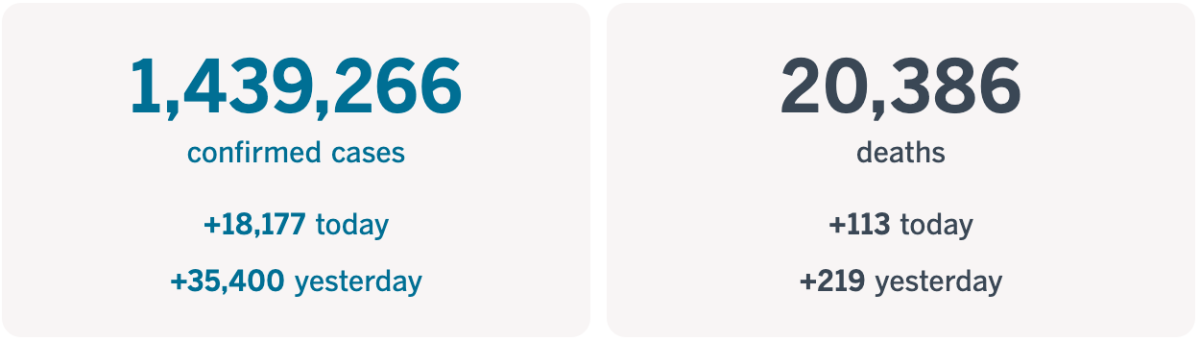
Track the latest numbers and how they break down in California with our graphics.
Across California
On Tuesday, the state logged a record 35,400 new coronavirus cases, and more Californians died from COVID-19 than any other day to date. The total of 219 just passed the previous single-day record of 214 logged on July 31, data compiled by The Times show.
This latest death toll marks a tragic milestone in a pandemic that is infecting and hospitalizing residents far faster than ever, and may also signal even higher death tolls to come. Prior to Dec. 4, there were only two days when the single-day tally of cases exceeded 200. In the last five days, they have done so twice.
The weekly average for deaths each day — 135 over the past week — is at an unprecedented high. A month ago, the state was averaging about 44 daily deaths. Close to 1,400 Californians have died from COVID-19 in the past 14 days alone, and the disease has killed more than 20,200 in the state since the pandemic began.
As California keeps setting new case records daily, hospital intensive care units are filling up. ICU capacity in Southern California dipped to 9%, and it was only 4.2% in the San Joaquin Valley. In the Sacramento region, it fell to 14.3%, forcing that area to abide by the new regional stay-at-home order starting at 11:59 p.m. Thursday. (ICU capacity was 20.9% in the Bay Area and 27.1% in Northern California.)
Officials expect cases and hospitalizations to continue to rise as more people who were infected over Thanksgiving develop symptoms. And they pleaded with residents to follow the new stay-at-home rules in effect for 84% of Californians. “Our message is: As much as you can, stay at home,” said Dr. Mark Ghaly, California’s health and human services secretary. “We know that it works. We know that we can bring our transmission rates down.”
Some good news for parents: California has reversed its decision to close playgrounds amid the surge. The updated state guidance, released Wednesday morning, says that “playgrounds may remain open to facilitate physically distanced personal health and wellness through outdoor exercise” — a sharp turnaround from the previous rules, which ordered them closed in regions where critical care services were being strained due to COVID-19.
While several aspects of the regional stay-at-home order have faced backlash since Gov. Gavin Newsom announced it last week, the playground closures were a particular source of ire for parents, especially as places like malls were allowed to remain open.
Officials in L.A. County, which had closed outdoor public playgrounds before the state’s order, said it would follow the state’s lead and let them reopen. “Play is crucial for childhood development. But low-income communities of color living in dense housing often do not have access to a yard,” L.A. County Supervisor Hilda Solis wrote on Twitter. “With distance learning, having access to public playgrounds is more important now than ever.”
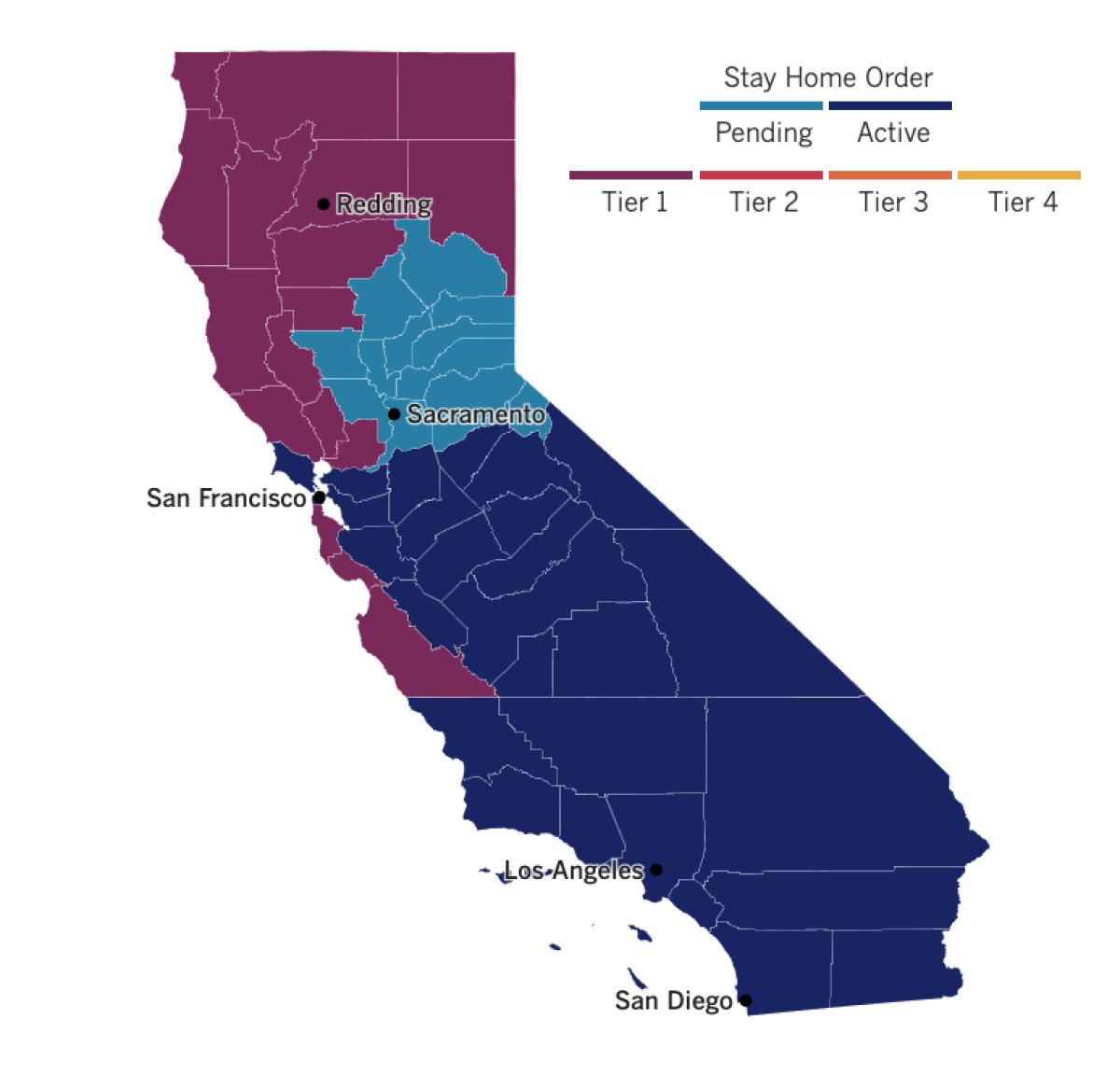
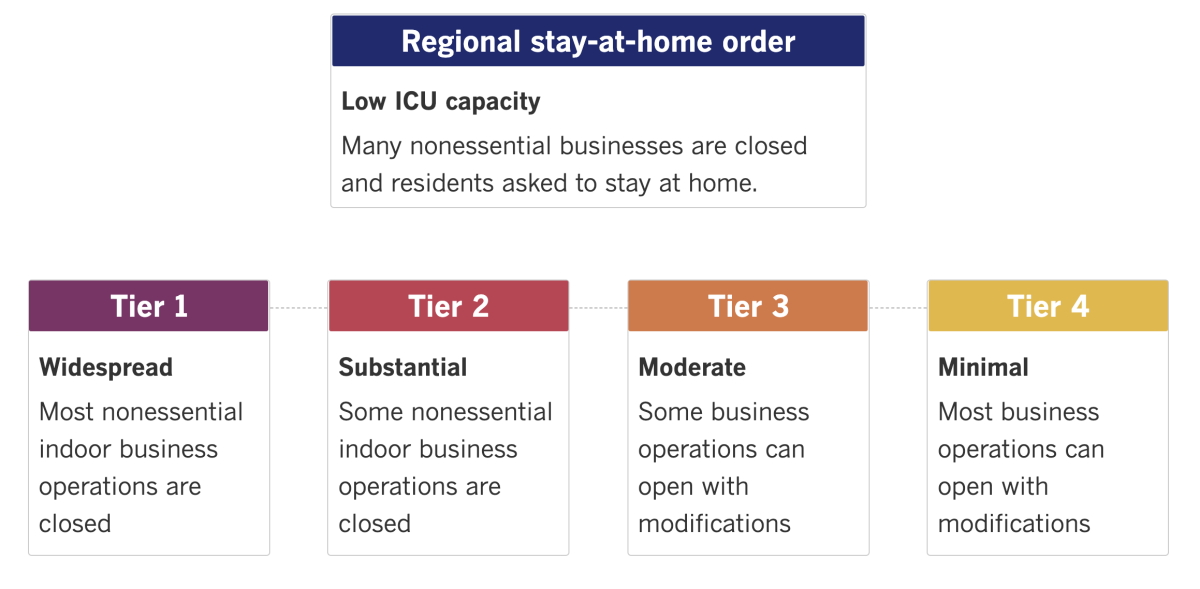
See the latest on California’s coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
Vaccine hesitancy is an issue far beyond California’s borders. As states gear up to start their own mass vaccination campaigns, a new poll finds that only about half of Americans are ready to get their COVID-19 shot when the time comes. The survey, from the Associated Press-NORC Center for Public Affairs Research, finds that roughly a quarter of adults aren’t sure if they want to get vaccinated, and another quarter or so say that they won’t.
Many of the undecided say they’re worried about safety and want to watch how the initial rollout goes. The problem is that such skepticism could actually hobble public health authorities’ efforts to protect residents against the virus.
Some of those on the fence may just need a push from a trusted public figure.
“If Dr. Fauci says it’s good, I will do it,” said Mary Lang, 71, of Fremont, Calif. She added: “Hopefully if enough of us get the vaccine, we can make this virus go away.”
President-elect Joe Biden called for urgent action on the COVID-19 pandemic Tuesday as he introduced his healthcare team, who will face major challenges in bringing the outbreak to heel. Biden laid out three pandemic-fighting priorities for his first 100 days in office: a call for all Americans to voluntarily mask up during that period, a commitment to administer 100 million vaccine shots and a pledge to attempt to reopen most of the nation’s schools.
“Out of our collective pain,” Biden said, “we are going to find a collective purpose: to control the pandemic, to save lives and to heal as a nation.”
The incoming commander-in-chief’s team will include California Atty. Gen. Xavier Becerra as his health secretary nominee and Jeff Zients, a businessman known for his crisis management skills who will become the administration’s coronavirus response coordinator. It will also include Dr. Anthony Fauci, the nation’s top infectious-disease expert, former surgeon general Dr. Vivek Murthy, who will be reassuming that role, and two other medical doctors.
A small fly in Britain’s vaccine ointment: U.K. regulators on Wednesday advised Britons with a “significant history” of allergic reactions to hold off on receiving the new Pfizer-BioNTech vaccine while authorities look into two adverse reactions that took place on the first day of the country’s mass-vaccination program.
The two people affected were staffers with the National Health Service who had a history of allergies, and both are recovering. Officials are investigating the cases to determine whether their reactions were linked to the vaccine.
They appeared to have experienced anaphylactoid reactions, which tend to involve a skin rash, breathlessness and sometimes a drop in blood pressure, rather than anaphylaxis, which can result in death. Still, health authorities said vaccinations should take place only in facilities with resuscitation equipment.
Pfizer and BioNTech said they were working “to better understand each case and its causes.” Late-stage vaccine trials found “no serious safety concerns,” the companies said.
German Chancellor Angela Merkel pushed for tougher restrictions on public life Wednesday and called on others to cut down on socializing as the country reported its highest single-day death toll of the pandemic.
Once seen as a model in Europe for keeping caseloads low, Germany is gradually moving toward a tighter lockdown, at least for a limited period after the Christmas holiday. New infections remain high in spite of a partial shutdown that began Nov. 2.
Germany’s national disease control center reported 590 coronavirus-related deaths over the last 24 hours, more than 100 higher than the previous record, itself just a week old. It also logged 20,815 new daily infections, compared with 17,270 a week prior.
While the country has now recorded close to 1.22 million cases, including 19,932 deaths, these numbers are still far lower than the caseloads and death tolls in other European nations including Britain, France and Spain.
Your questions answered
Today’s question comes from readers who want to know: What’s the science behind banning outdoor dining at restaurants?
Many folks have expressed frustration and confusion at the latest pandemic restrictions in California, including the closure of outdoor dining. An L.A. County Superior Court judge recently called on county public health officials to provide scientific evidence justifying their ban, following a legal challenge from a leading restaurant group.
The truth is that different experts have slightly different evaluations of the risk, probably because we’re still learning about the virus’ behavior. My colleague Deborah Netburn has taken a closer look at the science behind the county’s restrictions after speaking with a number of researchers and medical professionals, including Dr. Jeffrey Gunzenhauser, chief medical officer and director of the Disease Control Bureau at the L.A. County Department of Public Health.
Gunzenhauser said that eating outside is safer than eating inside, but that even outdoor dining has become much riskier than it used to be because so many more people are infected.
Other experts had a mixed view of the restriction. Dr. Peter Katona, a professor of medicine and infectious disease at UCLA, said the closure was justified given that people have to take their masks off to eat, increasing the risk of transmission.
On the other hand, Dr. Ravina Kullar, an infectious-disease expert in Santa Monica, argued that outdoor dining carries a lower probability of transmission, as long as tables are spaced out and masks are worn between bites (though it’s hard to imagine most diners actually do so).
For what it’s worth, Gunzenhauser said he understood folks’ confusion and frustration, in part because he and his colleagues feel the same way.
“The challenging part of this is we’ve been through a lot already, and people have been very hopeful that what we’ve done would be the worst of it,” he said. “We’re all trying to reconcile the conflicting emotions within ourselves — that hopefulness and the extreme disappointment. But the big question is, ‘What am I going to do?’”
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them.
Resources
Practice social distancing using these tips, and wear a mask. Here’s how to do it right.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




