Doctors suggest new, less threatening names for low-grade prostate cancer
A cancer diagnosis is scary. Some doctors say it’s time to rename low-grade prostate cancer to eliminate the alarming C-word.
Cancer cells develop in nearly all prostates as men age, and most prostate cancers are harmless. Treatments can lead to sexual dysfunction and incontinence.
Changing the name of low-grade cancers could lead more patients to skip unnecessary surgery and radiation.
“This is the least aggressive, wimpiest form of prostate cancer that is literally incapable of causing symptoms or spreading to other parts of the body,” said University of Chicago Medicine’s Dr. Scott Eggener, who is reviving a debate about how to explain the threat to worried patients.
The words “You have cancer” have a profound effect on patients, Eggener wrote Monday in the Journal of Clinical Oncology. He and his co-authors say fear of the disease can cause some patients to overreact and opt for unneeded procedures.
Others agree. “If you reduce anxiety, you’ll reduce overtreatment,” said Dr. David Penson of Vanderbilt University. “The word ‘cancer,’ it puts an idea in their head: ‘I have to have this treated.’”
In a shift that puts early detection of prostate cancer back on the agenda of middle-aged men and their doctors, a federal panel of experts is recommending that men ages 55 to 69 weigh the potential harms and benefits of prostate cancer screening and judge whether getting tested feels right to them.
Diagnosis sometimes starts with a PSA blood test, which looks for high levels of a protein that may mean cancer but can also be caused by less serious prostate problems, or even vigorous exercise.
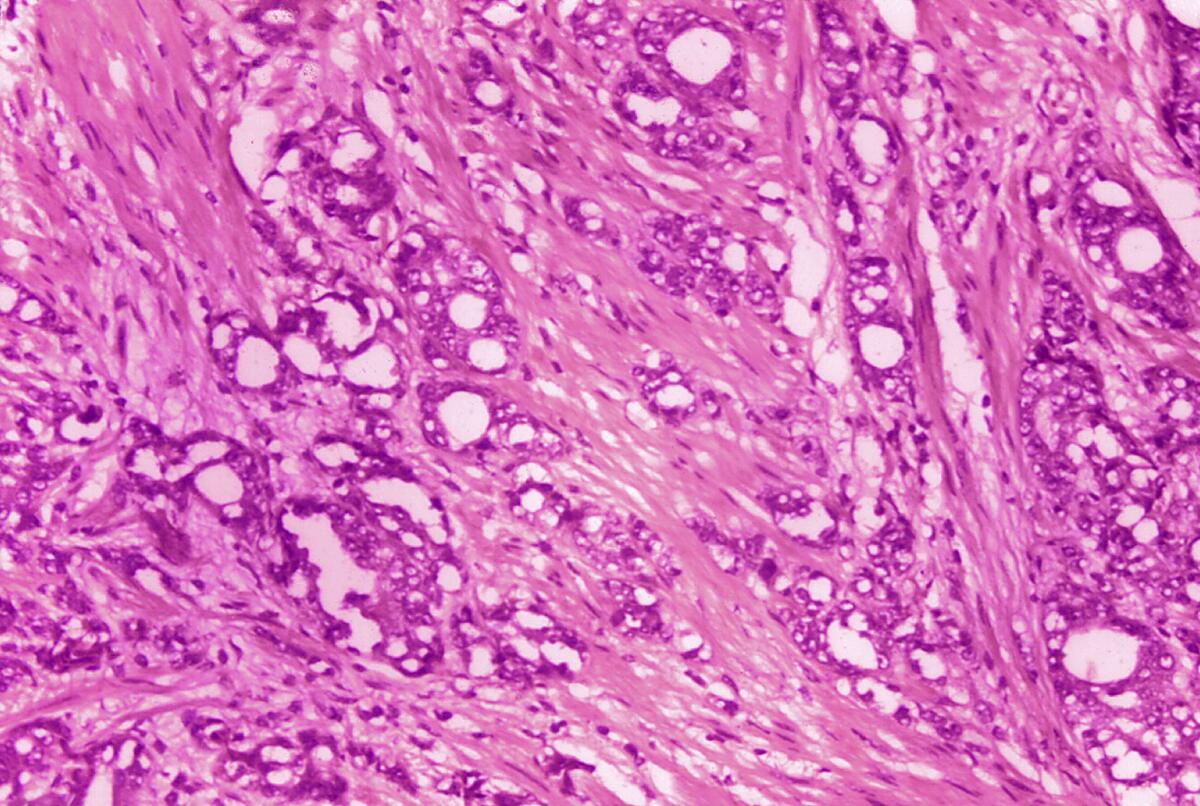
When a patient has a suspicious test result, a doctor might recommend a biopsy, which involves taking samples of tissue from the prostate gland. Next, a pathologist looks under a microscope and scores the samples for how abnormal the cells look.
Often, doctors offer patients with the lowest score — Gleason 6 — a way to avoid surgery and radiation: active surveillance, which involves close monitoring but no immediate treatment.
In the U.S., about 60% of low-risk patients choose active surveillance. But they might still worry.
“I would be over the moon if people came up with a new name for Gleason 6 disease,” Penson said. “It will allow a lot of men to sleep better at night.”
But Dr. Joel Nelson of the University of Pittsburgh School of Medicine, said dropping the word “cancer” would “misinform patients by telling them there’s nothing wrong. There’s nothing wrong today, but that doesn’t mean we don’t have to keep track of what we’ve discovered.”
About 34,500 Americans die from prostate cancer annually, according to the American Cancer Society.
Name changes have happened previously in low-risk cancers of the bladder, cervix and thyroid. In breast cancer, there’s an ongoing debate about dropping “carcinoma” from DCIS, or ductal carcinoma in situ.
Women were more likely to want surgery when they were told they had a type of breast cancer than when the diagnosis was a breast lesion or a group of abnormal cells — even though all three scenarios described the same disease.
In prostate cancer, the 1960s-era Gleason ranking system has evolved, which is how 6 became the lowest score. Patients may assume it’s a medium score on a scale of 1 to 10. In fact, it’s the lowest on a scale of 6 to 10.
What should it be called instead of cancer? Proposals include IDLE (for indolent lesion of epithelial origin) and INERRT (for indolent neoplasm rarely requiring treatment).
“I don’t really give a hoot what it’s called as long as it’s not called cancer,” Eggener said.
I don’t really give a hoot what it’s called as long as it’s not called cancer.
— Dr. Scott Eggener, a urologist at the University of Chicago
Steve Rienks, a 72-year-old civil engineer in Naperville, Ill., was diagnosed with Gleason 6 prostate cancer in 2014. He chose active surveillance, and follow-up biopsies in 2017 and 2021 found no evidence of cancer.
Calling it something else would help patients make informed choices, Rienks said, but that’s not enough: Patients need to ask questions until they feel confident.
“It’s about understanding risk,” Rienks said. “I would encourage my fellow males to educate themselves and get additional medical opinions.”







