- Share via
Two and a half years ago, my nose stopped working.
That’s when I realized how often smell comes up in daily conversation: “That Uber smelled weird,” or “that woman was wearing way too much perfume,” or “someone’s definitely smoking weed nearby.”
I have anosmia, a symptom of long COVID. I caught the virus early in the pandemic and had terrible symptoms, but after a week of bed rest, I was ready to resume my life. My nose wasn’t.
With the pandemic now well into its third year, anosmia — once an obscure problem — has become increasingly widespread.
Roughly 5% of people who experience smell loss during COVID-19 will develop long-term anosmia, according to Dr. Bradley J. Goldstein, an ear, nose and throat doctor at Duke University Hospital.
The impact is more drastic than most people realize.
“The sense of smell is one of our key sensory systems that is constantly providing information about our environment, about the world around us, to the brain,” Goldstein said. “A lot of that is happening sort of passively to us. We’re not always intentionally thinking about sniffing, but we’re constantly getting a lot of input.”
I’m now a junior in college, and I have no idea what my campus smells like. I am constantly afraid that I smell bad, that the food I’m about to eat is rancid or that my dorm might be on fire. I can’t remember the last thing I smelled.
“We tend to rely on vision and hearing perhaps a little bit more directly, but smell is still a really important sensory system. And when it’s not working, people really do realize that there’s something major sort of missing,” Goldstein said.
People love to tell me that having a dysfunctional nose can be good at times. And sure, I can cook broccoli in my studio apartment and use public bathrooms without gagging. I was unfazed during a 14-hour car ride from North Carolina to Louisiana with four boys (and their Moe’s Southwest Grill orders).
But then there are the other times. Like the gas leak in my dorm building — I was oblivious to the odor, watching TV, when my RA pounded on my door shocked to find that I had not already evacuated.
The sudden increase in the number of patients losing their sense of smell has had a major impact on odor researchers, as well.
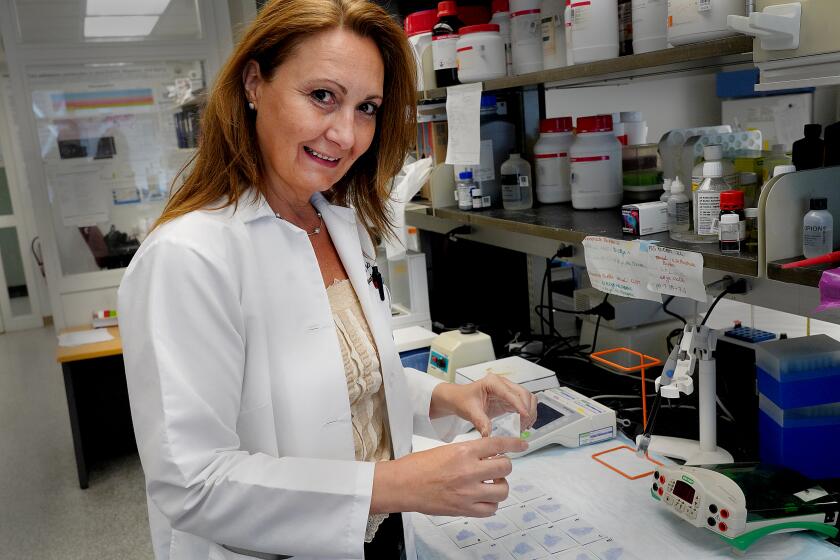
“It really radically changed the lives of many smell researchers that were doing something else and are now studying the effects of COVID,” said Dr. Danielle R. Reed, associate director of the Monell Chemical Senses Center in Philadelphia.
“It was really astonishing to suddenly be the focus of worldwide attention.”
Reed and her colleagues knew before the pandemic that viral infection could cause smell loss, but there wasn’t much attention paid to how or why. Now, answering those questions is paramount — and researchers have been thrown into the limelight.
Early on, Reed’s lab developed a test to try to standardize smell-loss diagnoses at doctors offices. It asks patients to locate smells on a sheet, rate their intensity and attempt to identify them. This way patients can know the severity of their conditions, and their doctors can easily measure improvement.
The L.A. Times wants to hear from long haul COVID-19 patients in California and their caregivers about how they’re navigating the challenges of their illness.
Now the lab is working on taking cells from tissue in the nasal cavity and growing them in a petri dish. They plan to expose these cells to SARS-CoV-2 and other viruses to learn why COVID-19 has a unique impact on smell.
“There are biological processes that we are working to understand. And if we can understand it, we can hope to correct it,” she said.
Researchers in Goldstein’s lab have undertaken similar work. Starting in 2020, they began to biopsy the nasal tissues of patients with post-COVID anosmia to see if they could uncover what was responsible for the loss of smell.
“We’re still learning more about what exactly is damaged or where exactly the damage is,” he said.
Still other researchers study how the virus attacks the olfactory nerve, which conveys smell sensations to the brain.
While researchers look for a cure, the internet has filled with suggestions — sometimes well meaning, but mostly ineffective.
People love to tell me about the latest cure they saw on TikTok. I’ve tried them all: the burnt orange trick, the flick to the back of the head trick, aromatherapy with essential oils and a daily nasal steroid. I went to Goldstein’s clinic to take a smell identification test and get a nasal endoscopy.
So far, there is no cure.
But there are ways to cope.
Early on, I’d smile and nod when people who didn’t know about my anosmia would ask me things, like to confirm that their candle from Bed Bath & Beyond smelled good. I was embarrassed to tell them that I really didn’t know. Like it somehow made me seem lesser.
“Oh crap, I’m sorry,” my Dad started saying every time he instinctively commented on a passing aroma.
But I actually like when people bring up surrounding scents.
“It’s OK, just describe it to me,” I’ll respond.
I want to know that the Subway sandwich shop across the street from my apartment still emits wafts of warm, strangely sweet bread. Or that the pasta my sister ordered for dinner made the whole table smell like truffles.
Sometimes when walking into a restaurant or store for the first time, I’ll say out loud, “What’s that smell?” just in case there is one for someone to tell me about. I don’t want to be left out.
I’ve learned that the English language is lacking in scent descriptors. Most of the time people just default to “good” or “bad.”
If they’re really trying, people will add a ‘y’ onto the end of another word. Earth-y. Mint-y. Fruit-y. These are better than “good,” but still hard for me to wrap my head around. (Tropical fruity and wild berry fruity are two very distinct scents — that, I remember.)
At some point, I started saying “compare the smell to something” rather than “describe it.” It’s much easier for me to imagine a scent when someone likens it to, say, a wet dog or strawberry Jell-O.
My close friends understand the need to say that bakeries we pass smell like caramelized sugar, and that college parties we attend smell like sweaty boys and old beer. Those are smells I know.
Luckily my sense of taste has not been dramatically affected. I’ve done blind taste tests with different potato chip flavors to confirm this.
A person can taste with a dysfunctional nose, Goldstein said. Sensations from tastebuds in the mouth are just one part of how we experience flavor. The mouth feel from sensory nerves and the airborne substances that find their way to olfactory cells in the nose “give you a lot of information about the chemical qualities of food,” Goldstein said.
“If someone totally loses their sense of smell, they’re missing a lot of that input,” he said. “Yes, they can still taste salty or they can still taste sour or bitter, but some of the other qualities that are mediated by the olfactory sensation are kind of missing.”
In my case, while I’m sure my taste is less refined than it was before I got COVID-19, the eating experience has never become a chore. I never had to rely on texture more than flavor or douse my food in hot sauce to feel something.
That sort of loss is just one of the additional problems that some people who have lost their sense of smell deal with. For some, the impact can include depression and anxiety, Reed said.
“Nobody really wants to talk about the mental health aspect of it,” she said. “But that is definitely something that comes up over and over again.”
Chrissi Kelly, now an advocate in Britain for treatment of smell disorders, lost her smell following a sinus infection in 2012. Soon after, she began to experience intense depressive effects.
“I was unprepared for that and didn’t really know where to go for advice,” Kelly said. “It really did change my life. It was just a very, very dark time for me.”
Kelly founded AbScent shortly after her diagnosis, when anosmia was not as well known. The organization, which provides support and information to those affected by smell disorders, has seen rapid growth with the onset of COVID-19. Before the pandemic, it had around 1,500 members; now it serves more than 85,000 people worldwide.
Explaining the condition to those who are unaffected is one of the most challenging parts of advocacy, Kelly has found.
“You just don’t even know where to begin,” she said. “I think it’s because smell is so elemental to all organisms. And therefore, imagining life without that is just unthinkable. It’s like saying, ‘OK, I’d like you to imagine a life without gravity. Or how about you imagine a life without time?’”
It’s hard to describe “how weird it is, how suffocating it is,” she said.
“Recovery is chaotic,” Kelly tells AbScent members. Anosmia can change from day to day and requires patience. In her case, recovery took eight years.
As for me, I’ll catch whiffs here and there. A hint of my dog’s food when I pour it into her bowl or a whisper of smoke from a passing cigarette.
Whether they are phantom scents, I can’t say. But they make me hopeful.
Recently, I was sitting in bed with my computer when something made my nose wrinkle. I ignored it at first. Then I remembered two slices of bread I had put in the toaster 15 minutes earlier.
When I ran into the kitchen, I found two smoking, charred squares. A few expletives later, while tossing the slices in the trash, I audibly gasped.
I hadn’t jumped out of bed because I saw the burning bread. I hadn’t heard the machine beep. I smelled the smoke. Or perceived it with some other developing sixth sense.
Either way, it was the most excited I’ll ever be about burnt toast.
Dr. Maura Boldrini is studying the brains of people who died of COVID-19 to better understand how it causes neurological symptoms.