Nursing home COVID-19 cases rise four-fold in surge states
WASHINGTON — Despite the Trump administration’s announcement of efforts to erect a protective shield around nursing homes, coronavirus cases are surging within facilities in states hard hit by the latest onslaught of COVID-19.
The administration has allocated $5 billion to nursing homes, shipped nearly 14,000 fast-test machines with a goal of supplying every facility and tried to shore up stocks of protective equipment. But the data call into question the broader White House game plan, one that pushes states to reopen while maintaining that vulnerable people can be cocooned, even if the virus rebounds around them.
“Trying to protect nursing home residents without controlling community spread is a losing battle,” said Tamara Konetzka, a nationally recognized expert on long-term care. “Someone has to care for vulnerable nursing home residents, and those caregivers move in and out of the nursing home daily, providing an easy pathway for the virus to enter.”
The global COVID-19 death toll surpassed 1 million, one measurement of a scourge that has ravaged lives and economies and evoked an era of plagues.
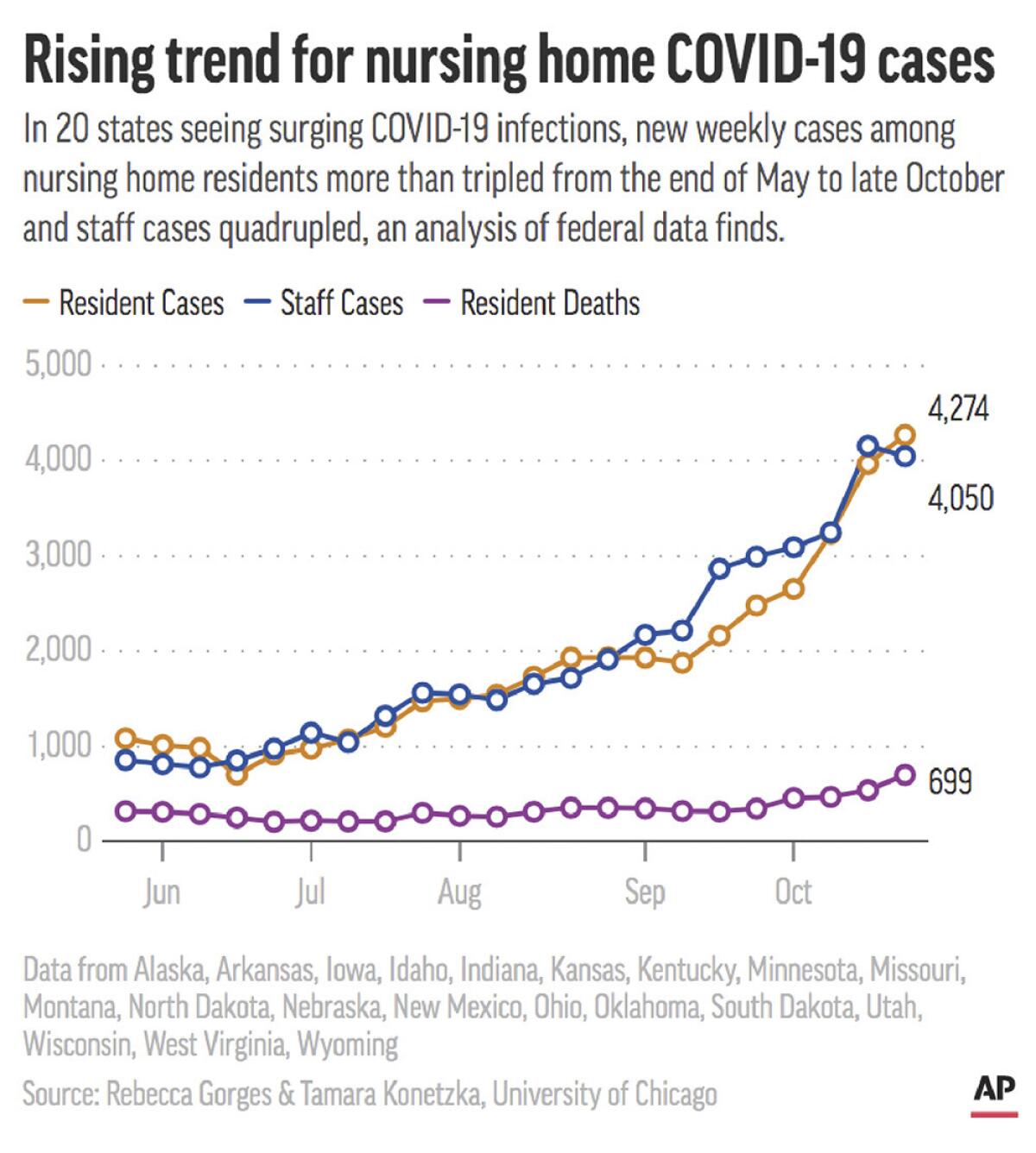
An analysis of federal data from 20 states for the Associated Press finds that new weekly cases among residents rose nearly four-fold from the end of May to late October, from 1,083 to 4,274. Resident deaths more than doubled, from 318 a week to 699, according to the study by University of Chicago health researchers Konetzka and Rebecca Gorges.
Equally concerning is that weekly cases among nursing home staff in surge states more than quadrupled, from 855 the week ending May 31, to 4,050 the week ending Oct. 25. That rings alarms because infected staffers not yet showing symptoms are seen as the most likely way the virus gets into facilities. When those unwitting staffers test positive, they are sidelined from caring for residents, raising pressures on remaining staff.
The nation is setting records for coronavirus cases heading into cold weather season when many experts expect the virus will be harder to contain. The seven-day rolling average for daily new cases stood at nearly 104,000 on Saturday, according to data from Johns Hopkins University.
Nursing homes and other long-term care facilities account for about 1% of the U.S. population, but represent 40% of COVID-19 deaths, according to the COVID Tracking Project.
In Fort Dodge, a manufacturing and transportation center in north-central Iowa, Julie Thorson said she knew she was in for a bad week when several employees at the Friendship Haven nursing home tested positive on Monday. As president of the senior living community, Thorson contacted the county health department. “They were basically not surprised because they’re seeing it all over the county,” she said.
Residents also started testing positive. As of Friday, the facility had 11 new cases among residents.
“I was thinking all night what’s worse: to have it hit and not know what you are getting into, or to prepare, prepare, and prepare, and then have it hit?” Thorson asked.
Responding to the study findings, the federal Centers for Medicare and Medicaid Services issued a statement saying that “the bottom line is that the COVID-19 pandemic’s effect on nursing homes is complex and multifactorial.”
The agency noted different ways the administration has worked to help nursing homes and said its focus now was on ensuring that residents and staff would “immediately” have access to a vaccine once approved. But it also added that facilities “bear the primary responsibility for keeping their residents safe.”
“Many times, the likely causes of nursing home outbreaks are simply nursing homes failing to comply with basic infection control rules,” the statement said.
But Konetzka said her research has shown that nursing home quality has no significant effect on cases and deaths once community spread is factored in. “It’s not like the high-quality facilities have figured out how to do things better,” she said. Other academic experts have reached similar conclusions.
Highly rated by Medicare, St. Paul Elder Services in Kaukauna, Wis., has had 72 COVID-19 cases among residents and 74 among staff, according to its Facebook page. The first case among residents was Aug. 19, and 15 have died, said the facility’s president, Sondra Norder.
“The outcomes are really not much different here than they were in New York back earlier in the pandemic,” Norder said. “It’s been called the perfect killing machine of the elderly, especially those who live in congregate settings.” Kaukauna is a small city about 100 miles north of Milwaukee.
The study, based on data reported by nursing homes to the government, also raised other concerns:
- For the week ending Oct. 25, about 1 in 6 nursing homes in surge states did not report having tested staff the prior week. Government requirements call for staff testing at least weekly in areas where the virus is spreading.
- During the same period, nearly 1 in 5 nursing homes reported shortages of basic protective supplies such as masks and gowns.
- Nearly 1 in 4 facilities reported a nurse staffing shortage.
Most of the states in the study are in the middle and northern tiers of the country.
The Commons, a senior living community in Enid, Okla., that includes a nursing home, is in a coronavirus hot spot. The oil and gas hub has a positive rate approaching 18%. A local mask mandate has twice been shot down, said Steven Walkingstick, chief executive of the Commons.
“From my standpoint, a mandate unfortunately is needed,” said Walkingstick. “I don’t want the government involved, but evidence has shown we are not going to do this voluntarily.”
Walkingstick said he believes the U.S. has gotten better at saving the lives of COVID-19 patients, but not at keeping the virus out of nursing homes.
Thorson, head of the Fort Dodge facility, said it takes a lot of effort to try to keep the virus out, and it’s demoralizing to see it break through.
“Don’t forget about us, because we are still here, doing the best we can in rural areas,” she said.
The 20 states analyzed in the study were Alaska, Arkansas, Iowa, Idaho, Indiana, Kansas, Kentucky, Minnesota, Missouri, Montana, Nebraska, New Mexico, North Dakota, Ohio, Oklahoma, South Dakota, Utah, Wisconsin, West Virginia and Wyoming. They were selected because they’re now seeing their highest hospitalization rates for COVID-19.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.











