FDA advisors endorse Janssen’s single-shot COVID-19 vaccine
- Share via
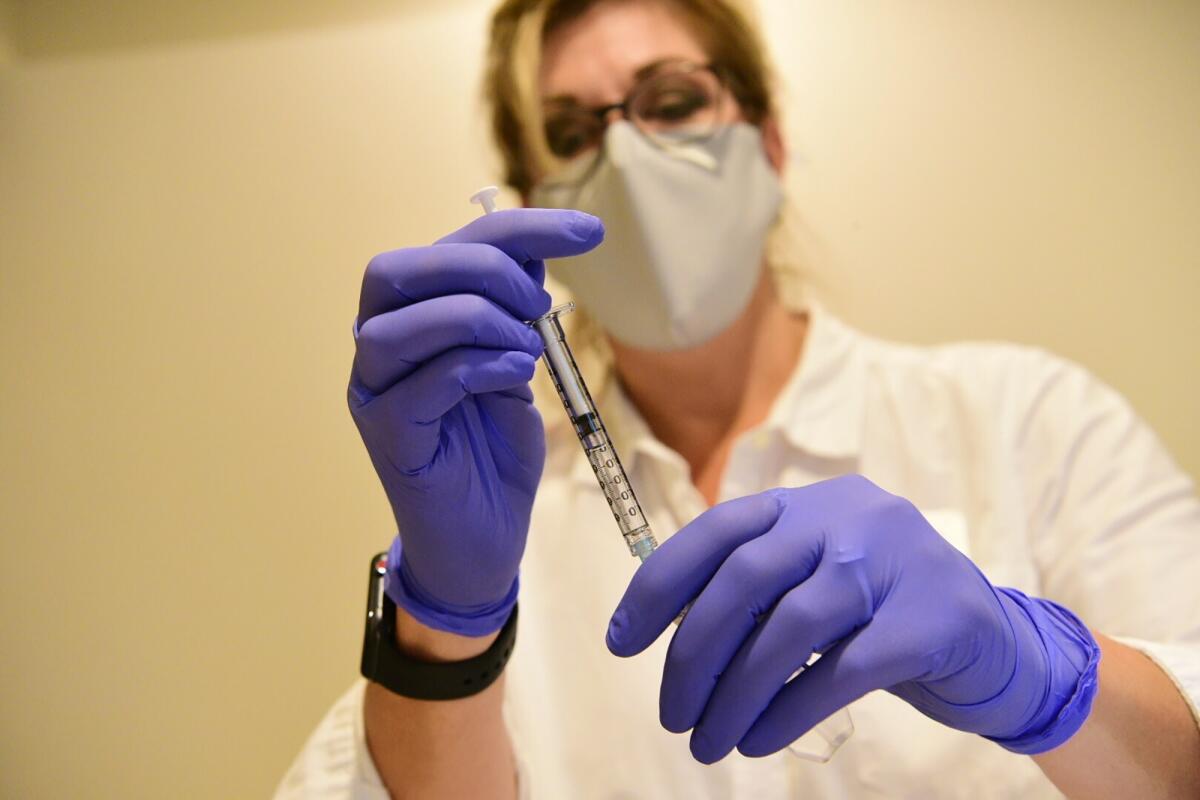
Federal authorities are all but certain to add a third COVID-19 vaccine to the U.S. arsenal, following a unanimous recommendation from a Food and Drug Administration advisory panel Friday that the agency authorize Janssen Pharmaceuticals to begin distributing its vaccine immediately.
Data reviewed by the panel suggest the vaccine — made by a division of Johnson & Johnson — are about 66% effective at preventing COVID-19 starting four weeks after the shot. Effectiveness against severe cases was about 85%.
The vaccine has the potential to be a game-changer, because unlike those already being used in the United States, it does not require shipping and storage at freezing temperatures and is administered in one dose instead of two.
All 22 independent experts on the advisory panel endorsed the vaccine for use in adults, saying the benefits outweigh any risks. The FDA isn’t required to follow that recommendation to grant emergency-use authorization, but it almost certainly will.
Authorization could come by Saturday, allowing shipments to begin as early as Monday.
The news comes just days after the U.S. death toll from COVID-19 surpassed 500,000.
“There’s an urgency to get this done,” said Dr. Jay Portnoy of Children’s Mercy Hospital, Missouri. “We’re in a race between the virus mutating and new variants coming out that can cause further disease and stopping it.”
About 22.6 million people in the United States, or 6.8% of the population, have been fully vaccinated using the two-dose regimens from Moderna and Pfizer-BioNTech, according to the Centers for Disease Control and Prevention.
At first, Janssen’s supplies will remain limited, but the company said it can deliver 20 million doses by the end of March and an additional 80 million by late June.
In the company’s Phase 3 clinical trial, 66 out of 19,306 people who got the vaccine developed the disease, compared with 195 out of 19,178 people who got the placebo.
The efficacy fell short of the results achieved by the two vaccines already on the market.
The one made by Moderna reduced the risk of developing COVID-19 symptoms by 94.5% among people who were tracked for a median of seven weeks after the second shot was administered.
Likewise, the Pfizer-BioNTech vaccine reduced the risk by 95% among people who were tracked for a median of two months after their second shot.
Researchers have said concerns about Janssen’s lower numbers are misplaced, adding that the most important metric is prevention of severe disease.
Vaccines shouldn’t be evaluated based on whether they prevent a cough, they said, but rather on whether they prevent hospitalization and death.
In the Janssen trial, there were no hospitalizations or deaths following the four-week period after the immunizations had taken full effect — even in South Africa and regions of Latin America where new variants of the virus have become common.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases and chief medical advisor to President Biden, called that “extraordinarily important” when the data were first released in January.
Researchers also said that comparing efficacy data can be misleading because the trials were conducted in different settings.
The U.S. trials of the Pfizer-BioNTech and Moderna vaccines were conducted in the summer and early fall of 2020, when several of the most concerning coronavirus variants were not yet circulating widely. Janssen did not begin its trials until September.
“It’s important that people do not think that one vaccine is better than another,” said Dr. Cody Meissner, a vaccine expert at Tufts University who served on the advisory panel.
The efficacy of the Janssen vaccine in clinical trials varied by region, most likely because of differences in the mix of variants in circulation.
It was 72% protective in the United States, 64% in South Africa and 61% in Latin America.
An analysis of the data suggested it worked well against the variant P.2, first identified in Brazil, but was slightly less effective against the variant first identified in South Africa, known as B.1.351.
Even if the vaccine is less effective than its competitors at preventing mild forms of illness, it has some significant advantages for the U.S. campaign to quickly inoculate as much of the population as possible.
The other vaccines must be stored frozen — the Pfizer-BioNTech between minus-80 and minus-60 Celsius in a specialized freezer — and used within a few days after thawing. Those requirements presented logistical problems and limited the types of facilities that can administer the shots.
The two-dose regimen also complicated the process of scheduling patients, who had to return for their second shots. The Janssen vaccine regimen of a single dose is twice as efficient.
During the trials, vaccine side effects were common, including injection site pain, headache, fatigue and muscle aches. Unexpected effects such as blood-clot-related conditions and ringing in the ears were reported in a handful of individuals.
A CDC panel is scheduled to meet Sunday to discuss how to make best use of the Janssen vaccine.
At the current pace, it could take at least until the fall to vaccinate 70% of the U.S. population, when the country could begin to achieve a level of herd immunity that makes it difficult for the virus to keep spreading. Until then, each new infection is a chance for the virus to mutate and for new variants to arise.
In that sense, the future of the pandemic and the likelihood of a safe return to normal life will depend largely on the public’s willingness to get the shots.
The Associated Press contributed to this report.







